Does Cupping Enhance Sports Performance?
Does Cupping Enhance Sports Performance?
By Romy Lauche PhD
When Michael Phelps won the gold medal at the Rio Olympics, the whole world psyched out – about those mysterious purple marks on his body. Purple dots or blotches, giant ‘love bites’, bruises, mysterious purple circles made the headlines, and cupping might again become a must-do. Manual therapists are probably familiar with Cupping, but this attracted media and social media uproar, with comments such as: fads, pseudoscience, superstitious, and load of hot air.
So what is cupping and how does it work?
Cupping is probably as old as mankind. In ancient times, when medicine as we know it now was not invented yet, cupping was used to cure many ailments. The traditional cupping was a bloody business as the skin was punctured or cut before the actual cupping. It was literately used to suck out the toxins that made men sick.
The modern (dry) cupping however is not nearly as archaic as it once was, and most cupping procedures do not involve the bloodletting anymore. One can even say that cupping has become a wellness intervention rather than a therapy, at least in the Western world. In Muslim cultures where cupping is part of the Prophetic Medicine the traditional bloody cupping is preferred still.
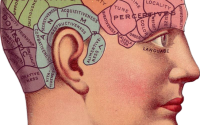
Cupping itself works with suction, and pretty much anything can be used, from special cupping devices to simple tea cups. The vacuum is created by fire or a mechanical pump, and the negative pressure will pull the skin into the cup. What happens than, has rarely been examined, but a few studies have shed some light into the hidden secrets of cupping.
The application of the cupping glasses will suppress microcirculation as deep as 3 cm into the skin and tissues (Emerich et al., 2014). First evidence of that has been reported in 1827 already, when Martin Barry examined the effects of subcutaneous poisoning in rabbits. When he applied the cupping glasses after subcutaneous arsenic injections nothing happened, but within moments after releasing the cups those poor animals would die of the poison (Chirali 2007). This indicates that microcirculation comes to a complete stop at the cupping site. When microcirculation is suppressed the tissue will be deprived of adequate oxygen supply, and this oxygen deficiency has been shown to increase lactate levels during and for up to several hours after cupping (Emerich et al., 2014). Such over-acidification bears the potential to damage nerves and tissues. As a result the body tries to resolve this state by dilating blood vessels to increase blood flow and oxygen supply (Modin et al., 2011; Hattori et al., 2002; Davis et al., 2011). This process is further amplified when small amounts of blood are forced to escape the capillaries and ‘leak’ into the surface tissues leaving the typical purple cupping marks. Blood clots in the surface tissues will initiate a ‘clean-up campaign’ of the body, as they need to be evacuated to avoid further cell damage.
What is the evidence?
There is only little evidence that dry cupping has beneficial effects. Small studies (Lauche et al., 2011, 2012, 2013; Kim et al., 2012; Cramer et al., 2011; Akbarzadeh et al., 2014; Markowski et al., 2014) found for example that cupping might help to improve neck and back pain, but the evidence is far from conclusive. At the current stage, there is also the possibility that the effects seen in those studies are largely driven by unspecific effects, known as placebo effects. A recent study has indeed found that the effects produced by cupping were comparable between the real intervention and the sham intervention in a sample of fibromyalgia patients (Lauche et al., 2015), however more studies are needed for conclusive judgement.
As for the effects of cupping in athletes there is literally no data available at all. So while Russian TV likens cupping therapy to doping (https://www.youtube.com/watch?v=V83CoTILr58) I fear it will not really improve athletes’ performance. It is even unclear if it can improve recovery from training, or muscle function. Nevertheless, the absence of evidence does not indicate ineffectiveness of cupping rather than little research interest in that topic so far. Let us hope that those celebrity situations help to spike interest in this widespread therapy to provide users and the critics with definite answers.
A word of caution!
Notwithstanding the above, cupping therapy might come with a risk. It is important that cupping is not (or only under close supervision) to be used for people who have bleeding disorders, or take blood thinning medication, on infected skin, wounds or in the presence of certain skin conditions. Cupping with fire requires extra caution, and bleeding cupping implies special consideration regarding hygienic standards. Thus the application of cupping by experienced and qualified personnel is vital for a safe and effective treatment.
Romy Lauche is a Chancellor’s post-doctoral research fellow at the Australian Research Centre in Complementary and Integrative Medicine (ARCCIM), University of Technology Sydney. Romy has a background and qualifications in psychology (MSc), and received her PhD in medical sciences.
References
Akbarzadeh M, Ghaemmaghami M, Yazdanpanahi Z, Zare N, Azizi A, Mohagheghzadeh A. The Effect Dry Cupping Therapy at Acupoint BL23 on the Intensity of Postpartum Low Back Pain in Primiparous Women Based on Two Types of Questionnaires, 2012; A Randomized Clinical Trial. Int J Community Based Nurs Midwifery. 2014; 2(2): 112-20.
Chirali, I. Traditional Chinese Medicine Cupping Therapy. 2nd edition. Philadelphia, PA: Elsevier Churchill Livingston, 2007.
Cramer H, Lauche R, Hohmann C, Choi KE, Rampp T, Musial F, Langhorst J, Dobos G. Randomized controlled trial of pulsating cupping (pneumatic pulsation therapy) for chronic neck pain. Forsch Komplementmed. 2011; 18(6): 327-34.
Davis MJ, Hill M A, Kuo L. 2011. Local Regulation of Microvascular Perfusion. Comprehensive Physiology. 161–284.
Emerich M, Braeunig M, Clement HW, Lüdtke R, Huber R. Mode of action of cupping–local metabolism and pain thresholds in neck pain patients and healthy subjects. Complement Ther Med. 2014; 22(1):148-58.
Hattori K, Tsuchida S, Tsukahara H, Mayumi M, Tanaka T, Zhang L, Taniguchi T, Muramatsu I. Augmentation of NO-mediated vasodilation in metabolic acidosis. Life Sci. 2002; 71(12): 1439-47.
Kim TH, Kang JW, Kim KH, Lee MH, Kim JE, Kim JH, Lee S, Shin MS, Jung SY, Kim AR, Park HJ, Hong KE. Cupping for treating neck pain in video display terminal (VDT) users: a randomized controlled pilot trial. J Occup Health. 2012; 54(6): 416-26.
Lauche R, Cramer H, Choi KE, Rampp T, Saha FJ, Dobos GJ, Musial F. The influence of a series of five dry cupping treatments on pain and mechanical thresholds in patients with chronic non-specific neck pain–a randomised controlled pilot study. BMC Complement Altern Med. 2011; 11: 63.
Lauche R, Cramer H, Hohmann C, Choi KE, Rampp T, Saha FJ, Musial F, Langhorst J, Dobos G. The effect of traditional cupping on pain and mechanical thresholds in patients with chronic nonspecific neck pain: a randomised controlled pilot study. Evid Based Complement Alternat Med. 2012; 2012: 429718.
Lauche R, Materdey S, Cramer H, Haller H, Stange R, Dobos G, Rampp T. Effectiveness of home-based cupping massage compared to progressive muscle relaxation in patients with chronic neck pain–a randomized controlled trial. PLoS One, 2013; 8(6): e65378.
Lauche R, Schwahn B, Spitzer J, Cramer H, Ostermann T, Bernardy K, Dobos G, Langhorst J. Efficacy of cupping therapy in patients with the fibromyalgia syndrome – a randomized sham-controlled controlled trial. Integrative Medicine Research, 2015, 4(1): 20.
Markowski A, Sanford S, Pikowski J, Fauvell D, Cimino D, Caplan S. A pilot study analyzing the effects of Chinese cupping as an adjunct treatment for patients with subacute low back pain on relieving pain, improving range of motion, and improving function. J Altern Complement Med. 2014; 20(2): 113-7.
Modin A, Björne H, Herulf M, Alving K, Weitzberg E, Lundberg JO. Nitrite-derived nitric oxide: a possible mediator of ‘acidic-metabolic’ vasodilation. Acta Physiol Scand. 2001; 171(1): 9-16.