Interoception: Some Suggestions for Manual and Movement Therapies
Interoception: Some Suggestions for Manual and Movement Therapies by Robert Schleip PhD.
The discovery of interoceptive receptors in human skin.
The established view is that touch is mediated by large-diameter, fast-conducting peripheral nerves and there are areas in the body that are more densely innervated and more cortically represented such as the finger tips and the lips. However recent findings showed that there is another purpose to touch that is more interoceptive than exteroceptive. Beside the well known cutaneous receptors for haptic perception human skin contains interoceptive C-fibre endings which trigger a general sense of well-being. The connections of these slowly conducting receptors do not follow the usual pathway of the pyramidal tract towards the proprioceptive areas in the brain. They rather project to the insular cortex, a key player in the regulation of interoception. This was recently discovered through experiments with patients lacking myelinated afferents. Whenever their skin was gently stroked, they responded with an increased sense of general well-being, although they were unable to detect the direction of stroking. Subsequent brain imaging studies revealed that the touch activated their insular cortex, while no activation was seen in proprioceptive brain areas. It is concluded that human skin contains special touch receptors, with a slow conduction velocity, which are part of a neurobiological system for social touch.
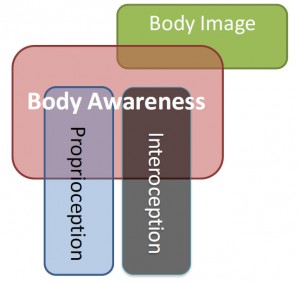
In manual and movement therapies, we have discussed the importance of proprioception, our sixth sense, the ability of our body to sense our relative position in space, be aware of its surroundings, and the sense in movement, the sense of effort, force, and heaviness. The awareness or how we perceive our own body can be quite variable (Figure 1). It is mostly linked to the ‘external’ signals to the body, such as how we look or touch our bodies or how our body acts in terms of biomechanical parameters. But body awareness can also be perceived by how we feel our body as a dynamic physiological organism from the inside. Recently a ‘new’ concept of interoception has been proposed. Body awareness relies on the representation of both exteroceptive, proprioceptive and interoceptive signals.
Figure 1. Body Image, Body Awareness, Proprioception & Interoception. Body awareness includes proprioception and interoception, whereas body image includes to some extent information on what our body looks like when observed from without (From Mosely, 2011).
So what is interoception?
The current concepts describe interoception as a sense of the physiological condition of the body, an ubiquitous information network used to represent one’s body from within. It is the ability to detect subtle changes in bodily systems, including muscles, skin, joints, and viscera (Dunn et al. 2010). It includes a range of physiological sensations, including: warmth, coolness, pain, tickle, itch, hunger, thirst, air hunger, sexual arousal, muscular activity, heartbeat, vasomotor activity, distension of bladder, distension of stomach, rectum or oesophagus, wine tasting (in sommeliers), and sensual touch.
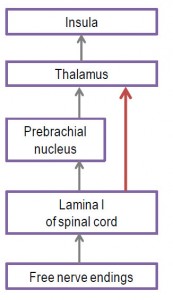
These sensations are triggered by stimulation of unmyelinated sensory nerve endings (free nerve endings) that project to the insular cortex rather than to the primary somatosensory cortex which is usually considered as the main target of proprioceptive sensations (Figure 2) (Berlucchi & Aglioti 2010). Feelings from these sensations not only have a sensory, but also an affective, motivational aspect and are always related to the homeostatic needs of the body. They are associated with behavioural motivations that are essential for the maintenance of physiological body integrity.
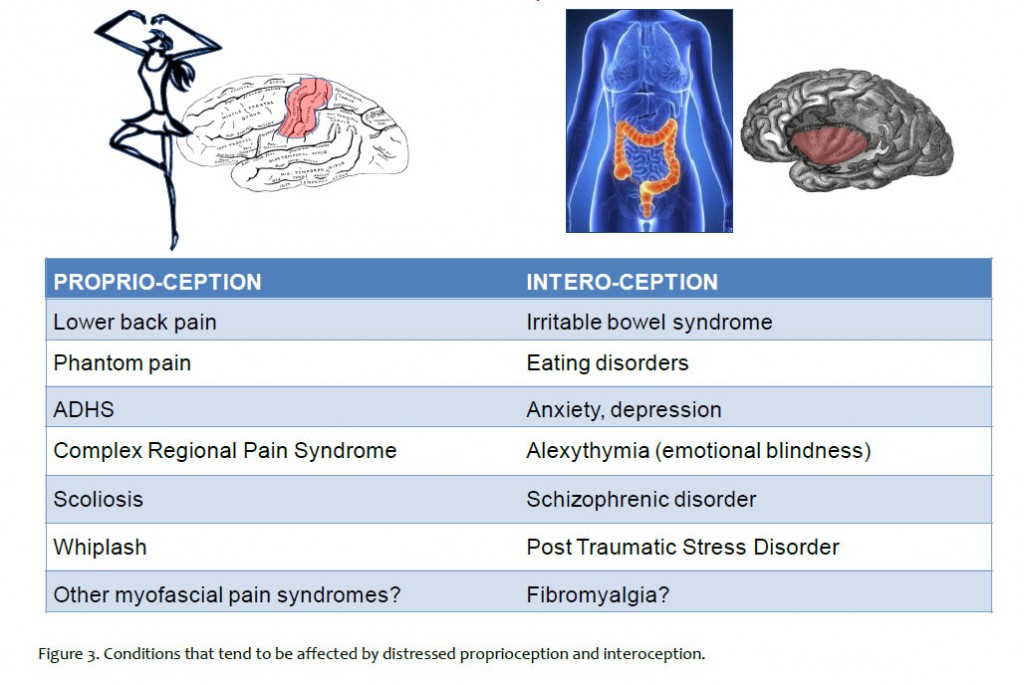
Distressed interoception and altered insular processing is associated with conditions such as irritable bowel syndrome, eating disorders, anxiety, depression, alexythymia (emotional blindness), schizophrenic disorders, Post-Traumatic Stress Disorder (PTSD), and possibly fibromyalgia. It has been proposed that the neural pathways associated with interoception may be considered as a potential correlate for consciousness (Craig, 2009). The sensory receptors for interoception are free nerve endings, most of which are located in fascial tissues throughout the human body. It is helpful to understand that proprioception and interoception are organized differently in the human brain and that very different afferent pathways are involved in them. Figure 3 shows some conditions that tend to be affected by distressed proprioception and interoception.
If applied with an open minded and careful attitude, it is an appealing thought that a more proprioceptive oriented therapeutic stimulation may work better for some conditions and a more interoceptive oriented approach for others.
Figure 2. A novel short-cut route for interoception in primates. In mammals, the main pathway of interoception starts with free nerve endings, which project to the lamina I of the spinal cord. From here they project to the prebrachial nucleus in the brainstem, and it is only from there that they are further projected to the insular cortex via the thalamus. In primates, however, there are additionally direct projections from lamina I to the insula via the thalamus. Primates therefore possess – as a novel phylogenetic acquisition – a more direct route between the afferent region for interoceptive sensations in the spinal cord and the insular cortex (red arrow).
Affective Touch
A recent and surprising addition to the list of interoceptive sensations is the sense of affective, sensual or pleasant touch. This discovery was triggered by examinations of a unique patient lacking myelinated afferents, slow stroking of the skin with a soft brush triggered a faint and obscure sensation of pleasant touch, although the patient was unable to recognize any stroking direction. Functional magnetic imaging showed that this vague sensation was accompanied by a clear activation of the insular cortex, while no activation was seen in the primary somatosensory cortex. (Olausson et al 2010).
Based on the innervation of primate skin and on subsequent studies with other patients it was concluded that there is dual tactile innervation of the human hairy skin: in addition to fast-conducting myelinated afferent fibres, there is a system of slow-conducting unmyelinated C tactile (CT) afferents that respond to gentle touch (Table 1). The C tactile afferents are a distinct type of unmyelinated, low-threshold mechanoreceptive receptors that are connected with neural interoceptive pathways. Those afferents have a slow conduction velocity (half to a second delay from stimulus to arrival in the brain). Since these receptors types have never been found in the glaburous skin (areas with lack of hair, mainly at palm of the hand and plantar of the foot) despite numerous micro neurographic recordings, it is assumed that they are only present in hairy skin. The cells are stimulated by gentle pressure on the skin and respond preferentially to gentle caressing stroke. C tactile afferents are connected to specific areas of the brain: the insular cortex, the posterior superior temporal sulcus, the medial prefrontal cortex and the dorsoanterior cingulate cortex, which are known to be activated by affective touch (McGlone et al., 2014). It is concluded that primate skin contains particular touch receptors which form a system for social touch that may underlie emotional, hormonal (for example oxytocin) and affiliative responses to caress-like, skin-to-skin contact between individuals (Figure 2). The profound importance of such a system for human health and well-being has long been indicated (Montague 1971), at least since the classical study of Harlow (1958) with baby rhesus monkeys that express affection for a surrogate mother in response to tactile comfort. This is reiterated by McClone et al. (2014) who suggested the “affective touch hypothesis”: the essential role of the CT system is to provide a peripheral mechanism for signalling pleasant skin-to-skin contact in humans, thereby promoting interpersonal touch and affiliative behavior.
Fascia as an Interoceptive Organ
In musculoskeletal tissues only a small amount of the sensory nerve endings are myelinated mechanoreceptors which are related to proprioception, such as muscle spindles, Golgi receptors, Pacini corpuscles or Ruffini endings. Predominantly, approximately 80% of afferent nerves, terminates in free nerve endings (Schleip, 2003). Termed ‘interstitial muscle receptors’ they are located in fascial tissues such as the endomysium or perimysium and are connected with either unmyelinated afferent neurons (then called type IV or C-fibres) or myelinated axons (type III or Ad fibres). Indeed 90% of these free nerve endings belong to the first group, to the slowly conducting C-fibre neurons. Functional magnetic imaging studies by Olausson et al. (2008) revealed that stimulation of these C-fibre neurons results in activation of the insular cortex (which indicates a clear interoceptive role of these receptors) and not of the primary somatosensory cortex which is usually activated by proprioceptive input.
A surprising conclusion from this is that the number of interoceptive receptors in muscular tissues by far outnumbers the amount of proprioceptive endings. Quantitatively, one could estimate that for every proprioceptive nerve ending in these tissues there are more than 7 endings which could be interoceptive receptors.
While some of these free nerve endings are thermoreceptors, chemoreceptors, or have multimodal functions, the majority of them do in fact function as mechanoreceptors, which means they are responsive to mechanical tension, pressure or shear deformation. While some of these receptors are high threshold receptors, it has been shown that a significant portion (approximately 40%) can be classified as low threshold receptors, which are responsive to light touch, even to touch as light as “with a painter’s brush” (Mitchell & Schmidt 1977). Most likely they are responsive to the gentle myofascial stretch by therapists.
Pain and Interoception
Camila Valenzuela-Moguillansky (2012) recently reviewed the relationship between chronic pain and body awareness. She presented evidences that showed the relationship between pain and exteroceptive body awareness is bidirectional: not only does pain change the body perception, but modifications in one’s perception of the body can modulate pain. In addition, she suggested that in order to give a full account of the relationship between chronic pain and body awareness it might be necessary to include the interoceptive sensorimotor system. While augmented attentive interoceptive sensitivity seems to be associated with increased myofascial pain perception, a mindfulness based interoceptive training can be helpful in the treatment of somato-emotional disorders such as anxiety or depression (Fjorback et al. 2013).
Pollatos et al. (2012) in an article published in Pain evaluated the relationship between interoception sensitivity and pain perception. This study was based on the idea that enhanced sensitivity to autonomic state is often accompanied by increased autonomic reactivity. As pain is made up of both sensory and emotional components, the authors investigated the relationship between pain and the ability to perceive physiological changes.
To evaluate interoception sensitivity, 60 healthy participants were asked to count their own heartbeat rate and compared it to actual heart rate count. Based on the data, participants were split into two groups: higher interoceptive sensitivity more accurate heart rate estimation) and low interoceptive sensitivity (more error in estimation). Then the participants were subjected to pain stimuli, using an algometer, cutaneous pressure pain was applied to the thenar eminence of the participants. Subjective pain intensity and unpleasantness was assessed along with heart rate variability and respiratory activity.
They observed significant relationship between heightened interoceptive sensitivity and enhanced sensitivity and decreased tolerance to pain. In other words, high interoceptive sensitivity participants had lower pain threshold and tolerance than low interoceptive sensitivity participants, they also rated threshold level stimuli as significantly more unpleasant. These effects were accompanied by a more pronounced parasympathetic decrease and a change in sympathovagal balance during pain assessment in the high, compared to the low, interoceptively sensitive group. The authors concluded that “better detection of internal signals and evoked bodily changes seems to increase pain perception for pressure pain”.
Manual Therapy and Interoception
Manual therapists when treating muscular tissues issues are mostly concerned with direct biomechanical effects on non-neural tissues or with the stimulation of specific proprioceptive nerve endings, such as muscle spindles, Golgi receptors, etc. However, based on the above information, manual therapists could target the interoceptive receptors and thus can trigger their related upstream effects much more effectively than what is commonly practiced.
Some of the interoceptive nerve endings in muscle tissues have been classified as ergoreceptors; they inform the insula about the work load of local muscle portions. Their mechanical stimulation has been shown to lead to changes in sympathetic output which increases the local blood flow. Stimulation of other interoceptive nerve endings has been shown to result in an increased matrix hydration, via an augmentation of plasma extravasation, i.e. the extrusion of plasma from tiny blood vessels into the interstitial matrix (Schleip 2003).
It would be really useful for the therapist to pay attention to the autonomic responses at each moment and to the limbic-emotional (or insular) response of the client, while monitoring the touch direction (plus its speed and magnitude) in such a manner that a profound change in local tissue hydration as well as other autonomic effects can be achieved. It would also be worthwhile to encourage a perceptual refinement and some verbal feedback from the client regarding his/her interoceptive perceptions. While proprioceptive sensations may be in the foreground during the application of strokes, those finer interoceptive sensations are usually easier to perceive in periods of at least several seconds of rest between different manipulative strokes. Subjective sensations of warmness, lightness/heaviness, spaciousness, density/fluidity, nausea, streaming, pulsation, spontaneous affection or a general sense of well being may be such interoceptive sensations that can be triggered by myofascial tissue manipulation. From the therapist’s perspective subtle changes in the client – such as an increased local tissue hydration, changes in temperature, in skin colour, in breathing, micro movements of the limbs, pupil dilation and facial expression can serve as valuable signals for physiological effects related to interoceptive processes.
Therapists which apply mechanical stimulation to visceral tissues, such as visceral osteopaths, should also profit from a larger recognition of interoception and related physiological as well as psycho-emotional effects. Recent discoveries concerning the richness of the enteric nervous system have taught us that our ‘belly brain’ contains more than 100 million neurons (Gershon 1999). Most of these are located either in the connective tissue zone between the inner and outer layers of the muscularis externa (Auerbach’s plexus) or in the dense connective tissue layer of the sub mucosa (Meissner’s plexus). Many of these visceral nerve endings are directly concerned with interoception and are connected via the “lamina 1-spinothalamocortical pathway” with the cortical insula, as described above. Considering that several complex disorders such as irritable bowel syndrome are associated with a disrupted modulation of insular responses to visceral stimuli, it is conceivable that a slow and careful application of manual forces to visceral tissues, if accompanied by a sense of safety and mindfulness of the client, could be useful if not ideal approaches for enhancing a healthy interoceptive self regulation.
Myofascial as well as visceral therapists should also not be surprised when encountering psycho-emotional responses or emotional release which may include changes in internal body perception, in self-awareness or affective emotions. These may be triggered by their stimulation of interoceptive free nerve endings in the skin, in visceral connective tissues as well as in muscular tissues.
Movement Therapies and Interoception
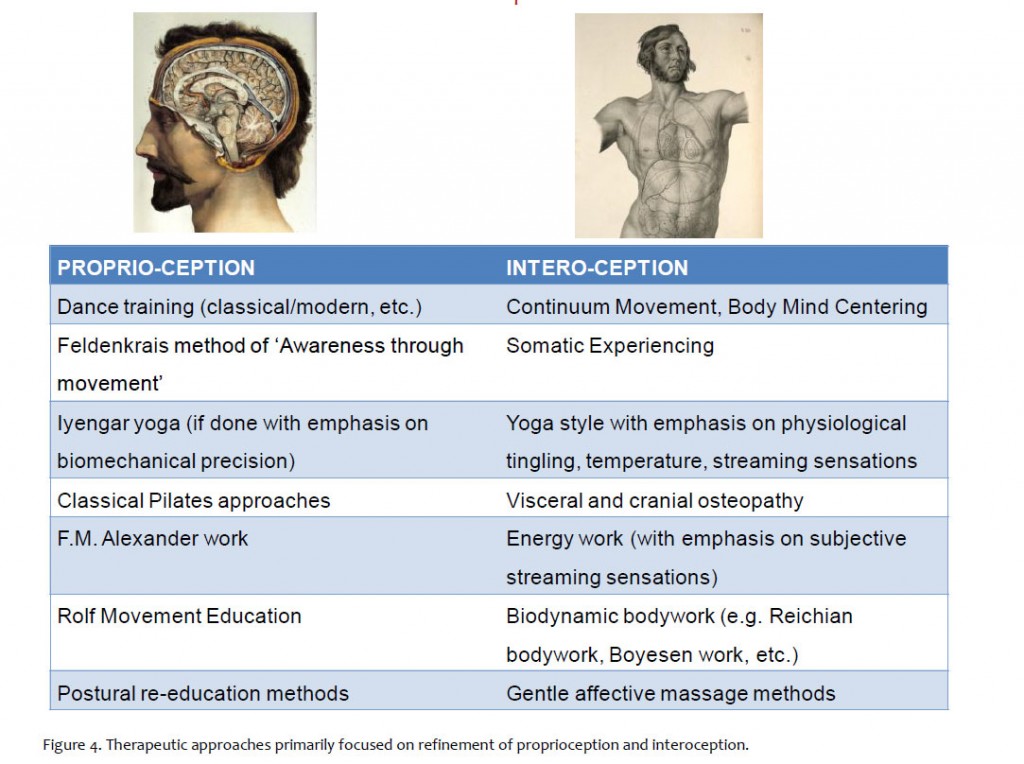
In competitive sports, the attention is often focused on achieving an external goal, and often it also focused on overriding internal sensations of discomfort, tiredness, etc. In contrast, complementary or alternative practices, such as Yoga, Tai Chi, Qi Gong, Pilates, Feldenkrais, Body Mind Centering or Continuum Movement, usually encourage a perceptual emphasis on finer sensations in one’s own body. However, depending on the focus of the individual teacher or respective school, the internal perception is sometimes directed almost entirely towards proprioceptive refinement. For example, a student of such training approaches may learn to feel minute movements of individual vertebrae or to control their lumbar lordosis within a multitude of loading situations. Nevertheless they may remain an ‘interoceptive moron’, e.g. unable to differentiate visceral sensations from signs of an empty stomach, of stage fright oriented ‘butterflies’, of empathy driven ‘gut feelings’ about another person’s dilemma, which may simply be an acute gastritis.
In contrast some teachers of these practices also include a skilled fine-tuning the student’s perception for interoceptive sensations (see Figure 4). This may include emphasizing sensations such as a subtle tingling under the skin, sensation of a general or localized warming, a subjective sense of internal spaciousness, a feeling of aliveness, an inner silence, an emotional ‘home coming’, or a meditation like change in general self awareness. For example gravity oriented changes in body positions, such as some upside-down postures in yoga practices, could easily trigger new and interesting (and hopefully unthreatening) sensations in visceral ligaments, which can foster interoceptive refinement. Given the recent research indications for a close correlation between disrupted interoception with many psycho-emotional disorders, such as irritable bowel syndrome, anxiety or post-traumatic stress disorder, it is plausible that some of these movement practices may have a strong therapeutic potential. Typically these therapeutic practices foster an attitude of inner mindfulness, of refining ‘internal listening skills’, and they frequently alternate brief periods of active motor attention with subsequent periods of rest where the students pay attention to small interoceptive sensations within their body. Not surprisingly, some studies already indicate a positive health enhancing effect of such mindfulness-based therapies for a large number of common clinical conditions (Astin et al 2003).
References
Astin JA, Shapiro SL, Eisenberg DM, Forys KL (2003) Mind-body medicine: state of the science, implications for practice. J Am Board Fam Pract 16: 131-147.
Berlucchi G, Aglioti SM (2010) The body in the brain revisited. Exp Brain Res 200: 25-35
Craig AD (2002) How do you feel? Interoception: the sense of the physiological condition of the body. Nat Rev Neurosci 3: 655-66
Craig AD (2003) Interoception: the sense of the physiologically condition of the body. Curr Opin Neurobiol. 13: 500-505.
Craig AD (2009) How do you feel-now? The anterior insula and human awareness. Nat Rev Neurosci 10: 59–70
Dunn BD, Galton HC, Morgan R, et al. (2010). Listening to your heart. How interoception shapes emotion experience and intuitive decision making. Psychol Sci 21 (12): 1835–1844.
Fjorback L, Arendt M, Ornbøl E, Walach H, Rehfeld E, Schröder A, Fink P (2013) Mindfulness therapy for somatization disorder and functional somatic syndromes: randomized trial with one-year follow-up. J Psychosom Res 74(1): 31-40.
Gershon MD (1999) The second brain. Harper Perennial, New York.
Harlow HF (1958) The nature of love. Am Psych 13: 673-689.
Montague A. (1971) Touch: the human significance of the skin. Harper & Row, New York
McGlone, Francis, Johan Wessberg, and Håkan Olausson (2014) Discriminative and Affective Touch: Sensing and Feeling. Neuron 82.4 : 737-755.
Mosely, L. How should we measure body awareness? Body In Mind. http://www.bodyinmind.org/how-should-we-measure-body-awareness/
Olausson HW, Cole J, Vallbo A, McGlone F, Elam M, Krämer HH, Rylander K, Wessberg J, Bushnell MC (2008) Unmyelinated tactile afferents have opposite effects on insular and somatosensory cortical processing. Neurosci Lett 436: 128-132.
Olausson H, Wessberg J, Morrison I, McGlone F, Vallbo A (2010) The neurophysiology of unmyelinated tactile afferents. Neurosci Biobehav Rev. 34: 185-191
Pollatos, O., Füstös, J., & Critchley, H. D. (2012). On the generalised embodiment of pain: How interoceptive sensitivity modulates cutaneous pain perception. Pain, 153(8), 1680-1686.
Schleip R (2003) Fascial plasticity – a new neurobiological explanation. Part 1. J Bodyw Movem Ther 7: 11-19
Valenzuela-Moguillansky, C. (2012) Chronic pain disturbances in body awareness. Chilean Journal of Neuropsychology, 7(1) 26-38.