Response from Clinical Anatomist John Sharkey to article on frozen shoulder following anaesthaesia.
This is a most interesting observational cross-sectional study providing results that, while based on a small cohort of patients, calls into question the current assumptions concerning this painful and life impacting “syndrome”. Frozen shoulder is the lay term for the painful condition referred to as adhesive capsulitis. Frozen shoulder Pain is reported to be worse at night, and is aggravated by sleeping on the affected shoulder often leading to the patient waking up several times a night. The results identified in this observational study call for a larger investigation. As a Clinical Anatomist I have had a special interest in the topic of Frozen Shoulder, or adhesive capsulitis, for over three decades. The so-called adhesive capsulitis tends to afflict individuals who are aged 40 and over and is more predominant in diabetics and people who have suffered a stroke, thyroid disease, recent surgery or Parkinson’s disease.
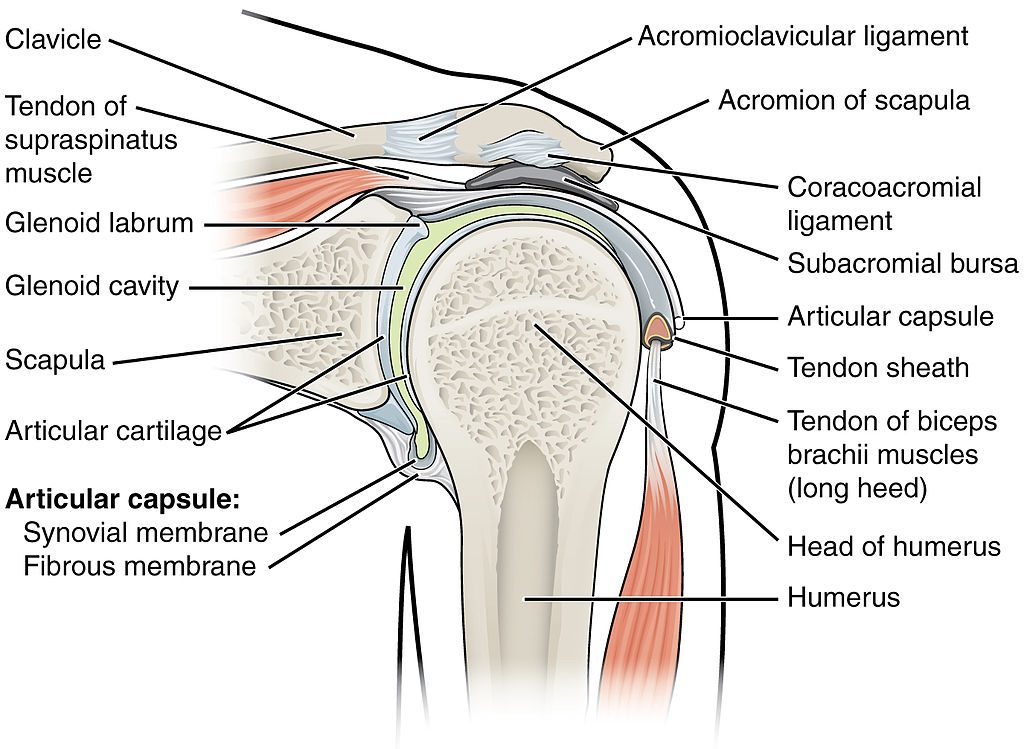
Adhesive capsulitis infers that the joint capsule of the shoulder has adhesions and inflammation thereby limiting the motion available at the shoulder or glenohumeral joint. While this condition is common, its underlying origin is not well understood. This condition is more common in females than in males. The non-dominant shoulder is more affected than the dominant shoulder.
The arm generally and the glenohumeral joint specifically is a highly mobile and complex anatomical structure providing the widest ranges of motion of any joint in the body. When I am teaching anatomy via cadaveric dissection I instruct students not to open the shoulder of cadavers until I am present at the table. In over thirty years of teaching anatomy and having performed many hundreds of dissections I have rarely found a truly adhered capsule on cadavers who were identified as having adhesive capsulitis when they were alive. This has led me to the conclusion that many people are “diagnosed” with a specific pathology that they simply do not have.
What this recent observational study demonstrates is that even when a true adhered capsule is present the joint can demonstrate near normal range of motion under anesthesia. What does this mean for practicing therapists in the clinical setting? This finding suggests that it is not the adhesion alone that restricts range of motion. Motion is possibly restricted by a protective neuromuscular “splinting” resulting in hypersensitivity (i.e. central sensitization) in the contractile and neural tissues resulting in pain on attempted movement. According to Latremoliere and Woolf , “Central sensitization represents an enhancement in the function of neurons and circuits in nociceptive pathways caused by increases in membrane excitability and synaptic efficacy as well as to reduced inhibition and is a manifestation of the remarkable plasticity of the somatosensory nervous system in response to activity, inflammation, and neural injury.”
A treatment plan must take into account the possibility that the true source of pain and limited range of motion is due to a protective or guarding increase in contractile tone. This observational paper also highlights the need to rule out other possible sources of pain and changes in range of motion, such as myofascial trigger points (Sharkey. 2017) or changes in fascial densification (Pavan, et al. 2014). While this brief response does not provide the opportunity to discuss this important topic in comprehensive detail it does provide the opportunity to highlight the need to investigate every option in terms of therapeutic interventions and not assume we have had the only word or the last word on frozen shoulders.
References
- Latremoliere A., Woolf C. J. (2009). Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J. Pain. 10, 895–926. 10.1016/j.jpain.2009.06.012 [PMC free article] [PubMed] [Cross Ref]
- Pavan, PG., Stecco, A., Stern, R., Stecco, C. 2014. Painful connections: densification versus fibrosis of fascia. Curr Pain Headache Rep. 18(8):441.doi:10.1007/s11916-014-0441-4
- Sharkey, J. 2017. The Concise Book of Dry Needling: A Practitioner’s Guide to Myofascial Trigger Point Applications. North Atlantic Press
John Sharkey MSc.
Clinical Anatomist (BACA)
Anatomical Society (Full Member)
Exercise Physiologist (BASES)
BioTensegrity Interest Group (Founding member)
Dry Needle Trigger Point Specialist
Senior Lecturer and Programme Leader MSc NMT University of Chester
johnsharkeyevents.com
Director
National Training Centre
16a St Josephs Parade
Dorset Street
Dublin D07 F6CR