Yoga and massage are associated with smaller placebo effects in chronic pain
Chronic pain is a common and debilitating condition that affects many people. Temporomandibular disorders (TMD) are a type of chronic pain condition that affects the jaw and can be difficult to treat. Complementary and Integrative Health Approaches (CIHA) are a range of treatments, such as yoga and natural products, that are used alongside or instead of conventional medicine to treat chronic pain. However, the efficacy of CIHA is not strongly supported by evidence, and it is possible that the benefits are due to placebo effects. The placebo effect involves distinct neurobiological and physiological mechanisms that can activate pain relief.
Since placebo effects can be seen as a form of endogenous pain modulation, it is possible that CIHA works, at least partially, through placebo mechanisms.
A study from University of Maryland published in European Journal of Pain investigated the relationship between the use of Complementary and Integrative Health Approaches (CIHA) and placebo effects in chronic pain management.
The study used a cross-sectional design to examine the relationship between self-reported use of CIHA and responsiveness to experimentally-induced placebo hypoalgesia, but did not investigate the efficacy of CIHA.
The study involved 361 TMD participants. Participants completed a checklist to track their use of complementary and integrative health approaches (CIHA), which was divided into three categories: physically oriented mind-body practices (e.g. Yoga, massage, acupuncture), psychologically oriented mind-body practices (e.g. meditation, breathing exercise), and natural products (e.g. vitamins, supplements).
They were assessed for placebo hypoalgesia using a standard method that included verbal suggestions and conditioning cues alongside specific painful heat stimulation. Pain disability was measured using the Graded Chronic Pain Scale, while the use of CIHA was documented through a checklist administered during medical history.
Participants underwent a pain sensitivity test, which assessed pain threshold due to prescribed heat stimulations: medium pain level, and maximum pain tolerance in an ascending manner.
The study used a placebo manipulation involving a conditioning phase and a testing phase. In the conditioning phase, red and green screens were paired with high and low heat temperatures, respectively, to condition participants to associate the red screen with high pain and the green screen with low pain. In the testing phase, the temperatures for the red and green screens were switched to the same temperature which was lower than the red screens from the conditioning phase. Participants were told the study was testing a new pain intervention (sham TENS electrode) that would reduce pain by inhibiting the pain signal, and the sham electrode would be turned on and off randomly based on the color of the screen. Pain ratings for the red and green screens were used to measure placebo hypoalgesic effects.
The study found that the use of physically oriented mind-body practices (MBPs) by participants with temporomandibular disorders (TMD) was associated with slightly reduced placebo hypoalgesic effects compared to those who did not use such practices.
Additionally, the use of a greater number of physically oriented MBPs was associated with smaller magnitude of placebo effects. Specifically, the use of yoga and massage were found to significantly reduce placebo hypoalgesia. The use of natural pain products or psychologically oriented MBPs did not have a significant effect on placebo hypoalgesia. These findings were independent of individual variability in heat painful sensitivity.
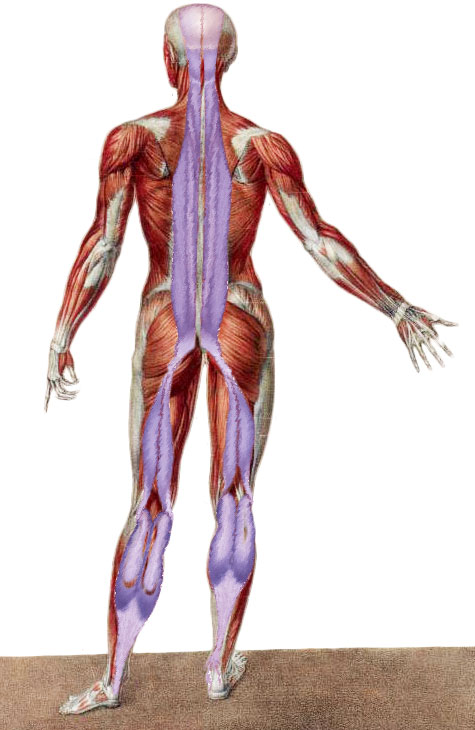
Physically oriented CIHA users, such as those who use yoga and massage, responded less to the placebo manipulation. Affective-based expectations mediated the relationship between the number of physically oriented CIHA and the magnitude of placebo effects. Chronic pain patients seek CIHA approaches independently of their pain disability. Those who suffer from chronic pain for more than 5 years are more likely to use physically oriented CIHA and natural products. The study suggests a potential interaction between the hypoalgesic mechanisms of physically oriented CIHA and placebo effects.
The authors suggests that yoga require introspection and concentration, which may lead to a more accurate assessment of internal states, including pain. This may explain why yogis have a smaller placebo effect in response to heat-pain stimulation in laboratory studies. Regular practice of physically oriented MBPs may improve sensory input and decrease the impact of prior experiences of pain relief, making experimentally induced expectations less powerful in provoking placebo effects. Other studies also suggest that yoga users process pain signals differently, with increased bodily awareness and pain threshold. This highlights the importance of bodily awareness in exercise and the greater sensitivity of yoga users in a broader context.
The study also found that participants who used massage demonstrated smaller placebo hypoalgesic effects. Although no studies have investigated the link between massage and occurrence of placebo effects, previous studies have investigated massage in the context of pain modulation. Touch-based therapy, such as massage, can be viewed as one potential strategy to reorganize individuals’ somato-perceptual system, leading to an improvement in their ability to self-oriented concentration, and ultimately resulting in decreased placebo effects.
The study found that affective pain relief expectations, rather than cognitive ones, were important in mediating placebo effects. Participants who used a larger number of physically oriented mind-body practices exhibited placebo hypoalgesic effects only when mediated by higher affectively based expectations. This highlights the difference between logical thoughts and affective feelings in placebo effects, with affective components being critical mediators.
The study concluded that individuals who used physically oriented CIHA showed decreased placebo effects, possibly because they were better able to influence their psychophysical behaviors.