Evaluating the Efficacy of Ischemic Compression Therapy on Cervical Spine Mobility and Headache Characteristics in Migraine Patients
Migraine is a complex neurological condition that not only disrupts daily life but also often comes with painful musculoskeletal complications. Most migraine sufferers—up to 76%—experience neck pain, which may be linked to hypertonic muscles in the neck and shoulders, including the upper trapezius muscle. These muscle issues contribute to the physical discomfort associated with migraines and can severely limit neck movements.
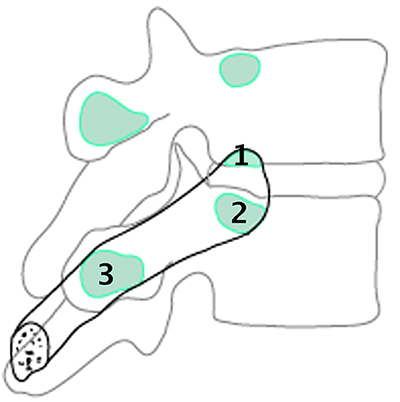
Research highlights that almost all migraine patients suffer from active myofascial trigger points, especially in the neck and shoulders. These trigger points disrupt muscle function and spinal mobility, which could worsen migraine symptoms.
A research published in BMC Musculoskeletal Disordersfocuses on exploring the efficacy of ischemic compression (IC) therapy on migraine sufferers, specifically targeting myofascial trigger points (MTrPs) that are commonly active in these patients. The study investigates whether this therapy can improve cervical spine range of motion (CS-ROM), reduce headache characteristics such as intensity, frequency, and duration, and influence CGRP (calcitonin gene-related peptide) concentrations in the blood.
The study included 83 participants diagnosed with various types of migraine. These participants underwent a series of IC therapy sessions, which involved applying pressure to MTrPs in the neck and shoulder regions. The outcomes measured were cervical spine mobility, headache features through self-reporting, and CGRP levels in blood samples.
Results indicated that IC therapy led to significant improvements in CS-ROM, especially in horizontal rotation and forward bending. It also reduced the intensity, frequency, and duration of migraine attacks. However, changes in CGRP levels were not significantly altered by the therapy, suggesting that while IC therapy effectively addresses mechanical and pain aspects of migraine, it does not significantly impact the underlying biochemical markers associated with migraine pathophysiology.
This study suggests that IC therapy could be a beneficial non-pharmacological treatment for reducing migraine symptoms and improving neck mobility, although further research is needed to fully understand its impact on biochemical pathways in migraine sufferers.
Thus, therapists need to consider both the neurological and musculoskeletal components of migraines in their treatment plans.