Understanding Neuroinflammation and the Role of the Sympathetic Nervous System: A Perspective on Manual Therapy
By Steven Goldstein
Neuroinflammation is a complex and multifaceted topic that continues to evolve as research advances. It is crucial to approach this subject with care, ensuring that the information presented is accurate and avoids perpetuating outdated or misleading narratives. While there are many experts who have contributed significantly to this field, it is important to acknowledge that our understanding of neuroinflammation is still developing. This article aims to explore the role of the sympathetic nervous system in modulating neuroinflammation and how manual therapy techniques, though not always evidence-based, can play a role in addressing these processes.
The Sympathetic Nervous System and Neuroinflammation
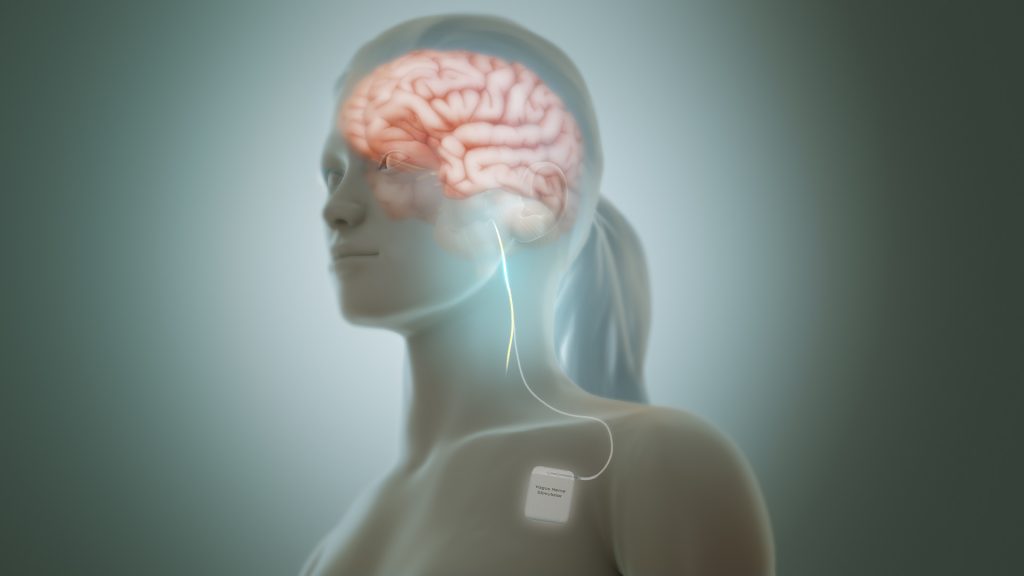
Michael Hamm, a prominent educator in the field, highlights the critical role of the sympathetic nervous system (SNS) in the modulation of neuroinflammation. Drawing from the research paper “Sympathetic Nervous System and Inflammation: A Conceptual View” by Wilfrid Jänig, Hamm emphasizes that the SNS can regulate inflammation in a tissue-specific manner. This means that the SNS is not merely a “fight or flight” system but also plays a nuanced role in managing inflammatory responses within the body.
When the autonomic nervous system (ANS) perceives a threat, it initiates a cascade of protective reactions, one of which is neuroinflammation. This response is part of the body’s innate mechanism to protect and heal itself. However, when the SNS remains overactive for extended periods—often seen in cases of chronic stress or trauma—it can lead to dysregulation and contribute to persistent inflammation. Conversely, the dorsal vagal branch of the ANS, which is responsible for immobilization and shutdown responses, can also become dysregulated, further complicating the body’s ability to return to homeostasis.
The Role of Manual Therapy in Modulating Neuroinflammation
While the mechanisms underlying manual therapy techniques are not always fully understood or supported by robust evidence, anecdotal and clinical experiences suggest that these methods can be effective in some cases. Techniques such as holding and supporting manual therapy applications are thought to help modulate the ANS, potentially reducing neuroinflammatory responses. These methods may work by calming the overactive SNS or stimulating the dorsal vagal system, thereby promoting a return to balance.
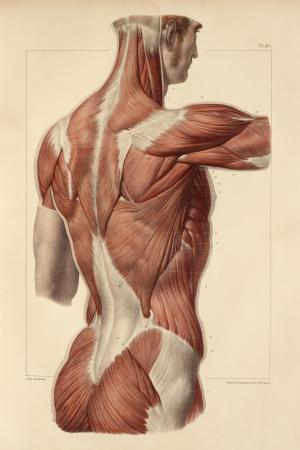
In my neurofascial mobilization course, it is essential to incorporate manual therapy applications. These techniques often combine perspectives from myofascial line models, orthopedic joint mobilization, and neural gliding principles. While the benchmarks used, such as neurodynamic tension tests, may have limitations, they provide a framework for assessing and addressing neural pathways. The reality is that these methods work some of the time, but not always—a reminder of the complexity of the human body and the individualized nature of treatment.
The Sympathetic Nervous System: Not the “Bad Guy”
It is important to reframe our understanding of the SNS and the ANS as a whole. These systems are not inherently “good” or “bad”; rather, they are designed to help the brain perceive and respond to threats, regulate bodily changes during stress or danger, and ultimately restore homeostasis. In healthy states, the SNS and dorsal vagal system work in harmony, allowing us to transition smoothly between states of activity and rest throughout the day. However, trauma or chronic stress can disrupt this balance, leading to prolonged sympathetic activation or dorsal vagal shutdown.
Addressing the Upper Extremity: A Holistic Approach
When focusing on the upper extremity, it is essential to consider the interplay between neural, joint, fascial, ligamentous, vascular, and lymphatic tissues. Each of these components interacts dynamically, and addressing one aspect often requires addressing the others. For example, techniques that focus on neural mobilization may help improve the gliding efficiency of nerves and reduce compression syndromes. However, whether these techniques directly reduce pain remains uncertain, as pain is a multifaceted experience influenced by numerous factors beyond tissue mechanics.
Conclusion
Neuroinflammation and the role of the SNS in modulating it are areas of ongoing research and debate. While our understanding is still evolving, it is clear that the SNS plays a vital role in regulating inflammatory responses in a tissue-specific manner. Manual therapy techniques, though not always supported by strong evidence, offer a practical approach to addressing neuroinflammation and promoting balance within the ANS. As educators and practitioners, it is our responsibility to continue learning, adapting, and refining our methods to better serve those we treat. By embracing a more inclusive and holistic perspective, we can move beyond reductionist models and work toward a deeper understanding of the interactions between the nervous system, inflammation, and manual therapy.
Join Steven Goldsteins’ workshop on Neurofascial Mobilisation: https://terrarosa.com.au/product/hands-on-workshops/ft-steve-goldstein/neurofascial-mobilisation/