Understanding Chronic Tendon Pain
Introduction
Chronic tendon pain (tendinopathy) is a prevalent and debilitating condition that impairs limb function, reduces physical activity, and diminishes quality of life. Despite its high prevalence, effective pharmacological treatments remain elusive due to an unclear understanding of its underlying pathophysiology.
Historically termed tendinitis, the condition is now recognized as tendinopathy, reflecting a clinical syndrome of pain, swelling, and impaired performance—without clear evidence of inflammation as the primary driver. Tendinopathy can affect over 1,000 tendons, with common sites including the rotator cuff (shoulder), Achilles tendon (ankle), and patellar tendon (knee). Risk factors include repetitive loading (sports or occupational activities), biomechanical abnormalities, metabolic disorders (diabetes, obesity), and certain medications (corticosteroids, statins).
Diagnosis and Current Challenges
Diagnosis relies on clinical assessment, including pain upon tendon loading and stretching. Imaging (MRI, ultrasound) may reveal structural abnormalities (e.g., tendon thickening, neovascularization), but these findings often do not correlate with pain severity. Many patients recover without resolution of imaging-detected pathology, suggesting that structural changes alone do not explain chronic pain.
Emerging Pathophysiological Insights
Recent research highlights key theories for chronic tendon pain:
Structural Changes Do Not Explain Pain
- Histological & Radiological Findings (e.g., collagen disorganization, neovascularization) are common in tendinopathy but do not correlate with pain.
- These changes are also found in asymptomatic individuals.
- Patients can recover from pain without reversal of structural abnormalities.
Neurogenic Pain Mechanisms – The most compelling evidence points to nerve ingrowth and neurochemical dysregulation as key pain drivers.
Key Findings on Neurogenic Pain in Tendinopathy
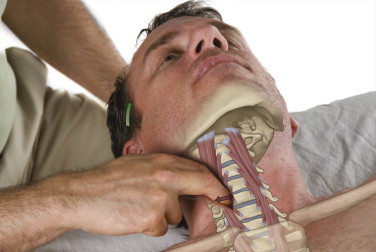
- Sensory Nerve Ingrowth: In healthy tendons, nerves are confined to the tendon sheath. Chronic pain is associated with abnormal nerve sprouting into the tendon proper.
- Pain Mediators & Receptors:
- Substance P (SP) and glutamate are elevated in painful tendons.
- NK1 (SP receptor) and NMDAR1 (glutamate receptor) are upregulated, increasing nociceptive signaling.
- Mast cells (immune cells) interact with nerves, releasing pro-inflammatory mediators (e.g., NGF, tryptase) that perpetuate pain.
- Neuro-Immune Cross-Talk: Glutamate and SP activate mast cells, creating a feedback loop that sustains inflammation and sensitization.
Implications for Treatment
Current evidence-based treatments (eccentric exercise, shockwave therapy) may work by modulating nerve activity rather than reversing structural damage:
- Eccentric Exercise: May regulate neurotrophic factors (NGF, BDNF), influencing nerve plasticity.
- Shockwave Therapy (ESWT): May induce selective sensory nerve fiber denervation, reducing pain.
Potential Future Therapies
Given the neurogenic basis of tendon pain, emerging pharmacological targets include:
- NGF inhibitors (e.g., anti-NGF antibodies) – Block nerve sprouting and pain sensitization (though safety concerns exist).
- NK1 receptor antagonists – Target SP-mediated pain pathways.
- Glutamate/NMDA receptor blockers (e.g., topical ketamine) – May reduce peripheral sensitization.
Conclusion
Chronic tendon pain is driven by neurogenic mechanisms (nerve ingrowth, upregulated pain receptors, and neuro-immune interactions) rather than structural degeneration alone. Therapists should consider:
- Mechanism-based approaches (eccentric loading, shockwave therapy).
- Emerging pharmacological targets (NGF, glutamate, SP pathways).
- Individualized management addressing intrinsic (biomechanics, metabolic health) and extrinsic (loading patterns, medications) risk factors.
By shifting focus from structural pathology to pain mechanisms, clinicians can better tailor interventions for chronic tendon pain.
Key Takeaway: Chronic tendon pain is not just a “wear and tear” condition—it’s a neurogenic disorder requiring targeted, multimodal treatment.