Immediate Effects of Myofascial Release Treatment on Lumbar Microcirculation
The thoracolumbar fascia (TLF) is a complex structure in the dorsal trunk region that connects muscles and transmits forces. It has been implicated in nonspecific low back pain and limited range of motion due to its mechanical properties. Inflammatory processes within the TLF can lead to thickening, densification, and fibrosis, and recent studies suggest that morphological differences in TLF characteristics are critical factors in the development of nonspecific low back pain.
Recent studies have shown that the TLF has extensive sensory innervation and that morphological differences, such as echogenicity and disorganization, may contribute to sensory disturbances and pain.
De Coninck et al. developed a scoring scheme of ultrasound images to evaluate the morphological characteristics of the TLF , the score is from 1 = “very disorganized” to 4 = “very organized”. They found that even inexperienced medical practitioners could reliably assess the organization of the TLF.
Blood circulation is critical for maintaining the function of the TLF, and a decrease in blood flow may trigger fascial degeneration. Fascial restrictions can also decrease blood flow. Physical activity, age, BMI, and neurological factors affect fascial blood flow and oxygen saturation. Postganglionic sympathetic fibers innervate the arterioles of the TLF and can act as vasoconstrictors.
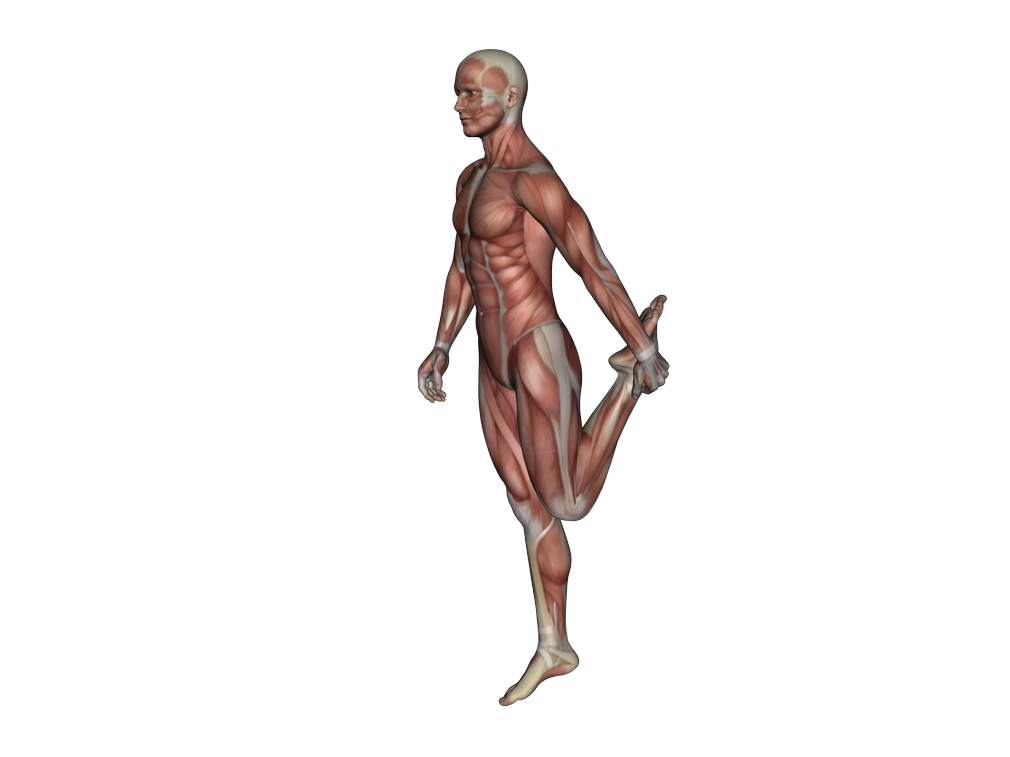
Mechanical stimuli, such as myofascial release treatment, can lead to vasodilation by increasing capillary permeability. Blood circulation is an important variable in studying the relationship between physical activity, BMI, TLF morphology, and manual treatment. MFR treatment involves low force, slow speed mechanical shearing of the myofascial tissue, which is believed to result in lasting changes in fascial morphology and hydration. This method can trigger neuromuscular and neurovascular reflexes through numerous free nerve endings. Thus a new study specifically looked at the effects of MFR treatment on the blood microcirculation of TLF in vivo.
The study was published in Journal of Clinical Medicine, conducted by Department of Sports Medicine, Institute for Human Movement Science, Faculty for Psychology and Human Movement Science, University of Hamburg. It was a single-blind, randomized, placebo-controlled trial. Thirty pain-free subjects (40.5 ± 14.1 years) were randomly assigned to two groups treated with MFR or a placebo intervention.
The study found that myofascial release (MFR) treatment had a significant positive effect on blood flow (BF) in the thoracolumbar fascia (TLF) compared to a placebo (PLC) group. Bloodflow increased by 31.6% in the MFR group and decreased by 15.4% in the placebo group. The blood flow continued to increase in the MFR group during the 60-minute follow-up, while it remained relatively constant in the placebo group. The increase in blood flow likely improved oxygen and erythrocyte supply in the myofascial tissue. MFR treatment may stimulate free nerve endings with mechanoceptive, nociceptive, autonomic, and vascular functions in the fascial tissue, while the much gentler touch of PLC treatment likely affects only skin receptors.
The authors hypothesised that circulatory restrictions could lead to hypoxia-induced inflammation, which likely causes pain and impaired proprioceptive function and may contribute to the development of nLBP. MFR treatment could release fascial restrictions of blood vessels and free nerve endings.