A Journey in the Fascia Wonderland
An article is based on Robert Schelip’s talk at the 3rd World Fascia Congress in Vancouver 2012 which he called Alice in Wonderland- Getting curioser and curioser.
The scientific world and the clinician world rarely meet, and the fascia congress is one of the important events that tried to make scientists and manual therapists meet and starting to talk to each other. Most manual therapists or bodyworkers choose to be in the complementary and alternative group. The field is usually dominated by different schools, where the teachers or charismatic founders are regarded as the ‘knowledge’ authority. (Whitney Lowe called this The Sage on the Stage). The teachers are quite skilful but sometimes they made up an explanation of what they did, which can stretch a bit beyond from the scientific reality. For example Dr. Andrew Taylor Still, the founder of Osteopathy, and Dr. Ida Rolf, the founder of Rolfing. They have a very profound clinical knowledge, and they tried to explain what they are doing based on their knowledge at that time. Myofascial release was thought to be able to change the state of the ground substance from gel to sol, or able to loosen the cross links of the collagen fibre. But most of these theories or hypotheses came from their own intuition without any solid scientific proof.
The first fascia research congress held in Boston, in 2007, was covered by the prestigious Science magazine with an article titled “Cell Biology Meets Rolfing”, it described the opportunity but also the challenges of how scientists and clinician can meet and talk to each other. The two groups reach out to each other, with a hope to provide fruitful exchanges of ideas and experiences.
Robert Schleip has travelled from the clinician’s ‘alternative world’ to the Scientific world, by doing a PhD degree in fascia biology. Meanwhile scientists such as Tom Findley, a medical researcher, travelled to the clinician world by studying Rolfing for a few years. Robert compared himself as Alice who has travelled in the Scientific Wonderland, and came back and told his fellow therapists about the strange scientists and their experiments.
Robert gave three specific examples of what he as a clinician had been able to learn from the scientific world.
(1) Fluid dynamics
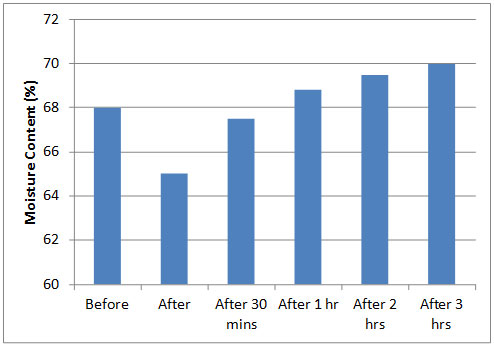
Water constitutes around 68% of the volume of fascial tissues. Fascia regulates fluid flow in the extracellular matrix, and fluid flow can cause fascial remodelling. A study conducted by Schleip and co-workers at the University of Ulm (Figure 1) showed that, in an in vitro study using fascia from animal, that during the tissue loading (fascia stretch) water is extruded from the tissue and this tends to contribute to a temporary decrease in tissue stiffness (i.e. tissue softening) immediately after the stretch. The findings also found that that after the stretch, the stiffness of the tissue increases and it also regains a gradual rehydration. This phenomenon is due to the behaviour of the ground substance in the extracellular matrix which prevented from absorbing fluid by the tension that fibroblast cells put on extracellular matrix fibres. When this tension is relaxed, the extracellular matrix can absorb fluid rapidly.
Figure 1. Changes in the mean water content of a porcine lumbar fascia before and following a 15 minutes stretch with a 4% strain (After Schleip et al., 2012)
The implication is that when Robert applied pressure through his elbow to the thoracolumbar fascia, he now paid more attention to the fluid dynamics, rather than only trying to melt the tissue or breaking up the fibrous tissues, or the mechanoreceptors. Now Robert started to work more gently and more slowly. We should now thinking not only about stimulating the mechanoreceptors or golgi tendon organ, but be aware of how the fluid moves.
Another research by Melody Swartz (from Lausanne, Switzerland) described how subtle change in fluid shear on cell culture has a profound change in the fibroblasts. Fibroblasts are most responsive to the detection of fluid shear – i.e. to the slow motions of the water around them – as sensed through their antenna-like cilia (soft tentacle). It is indicated that a large portion of the impact of collagen stretch is less due to the direct effect of transmission of that stretch to the cell membrane, but rather to the sensation of the fluid shear which is induced by the collagen fibre reorientation which is then sensed by the hair-like cilia.
This can be illustrated as follows: Imagine how much the hairy tip of a painter’s brush would bend if you move it at a steady speed through a fluid medium. Or imagine moving a finger through yoghurt. Both the speed as well as the viscosity of the fluid medium will influence the amount of shear. The clinical implication is that if you move very slowly at a constant speed through a dense tissue area (e.g. with the therapist’s knuckle or a foam roll), then the tiny cilia of the fibroblasts will be bent only very gently by the resulting fluid shear, and this seems to stimulate them to produce an enzyme (MMP-1) which starts to break down excessive collagen in the next few hours.
(2) A tool for evaluating the stiffness of tissue
Most palpation is subjective, and therapists cannot remember how ‘stiff’ is the tissue before and after treatment (or even a week after treatment). Therapists should have a more objective tool to measure the response. Robert suggested Myoton Pro, a myometer, a tool recently developed to measure tissue stiffness. The quantitative digital measurement provided by this myometer proved to be reliable and useful for assessing biomechanical properties of myofascial tissues. These tools create a constant pre-load of the soft tissue via a movable indentation probe, which is then rapidly released and the tissue response (damping oscillation) of the tissue is measured. This kind of tool will provide a more objective measurement how effective our treatment.
(3) The innervations of the lumbar fascia
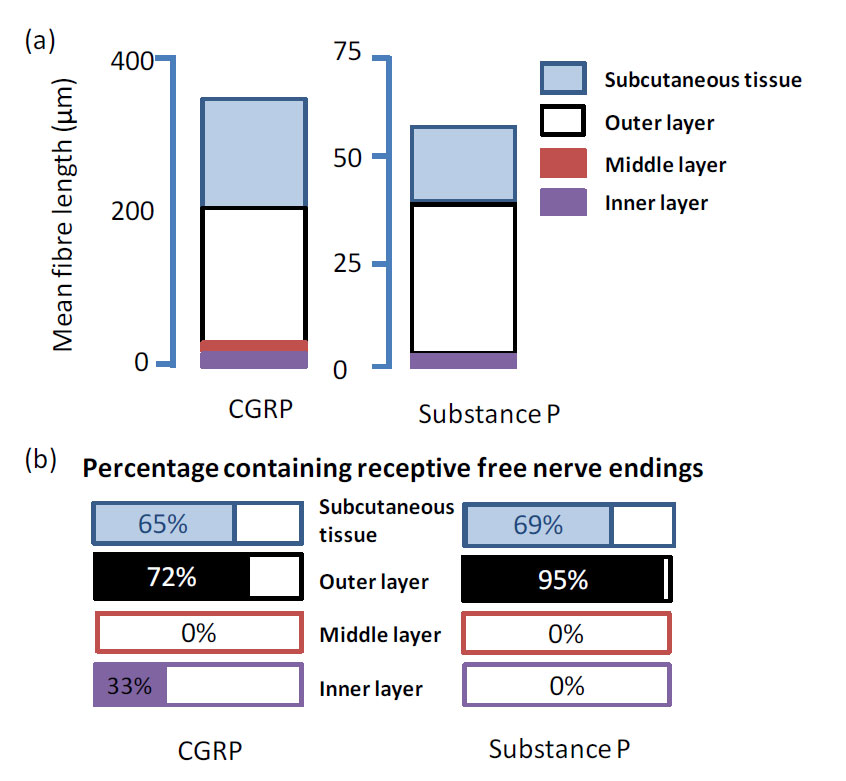
Sigfried Mense, in his lab in Heidelberg, Germany, showed that the thoracolumbar fascia is densely innervated. A recent study by Tesarz et al. (2011) published in Neuroscience, quantitatively evaluated the innervation of the thoracolumbar fascia (TLF). Using calcitonin gene-related peptide (CGRP) and substance P (SP)-containing free nerve endings, they quantified the amount of nerve endings in the TLF of rat. They showed that the TLF is a densely innervated tissue with marked differences in the distribution of the nerve endings over the fascial layers (Figure 2). They distinguished three layers: (1) Outer layer (transversely oriented collagen fibres adjacent to the subcutaneous tissue), (2) middle layer (massive collagen fibre bundles oriented obliquely to the animal’s long axis), and (3) inner layer (loose connective tissue covering the paraspinal muscles).
It is the subcutaneous tissue and the outer layer that showed a particularly dense innervations with sensory fibres. SP-positive free nerve endings, which are assumed to be nociceptive, were exclusively found in these layers. Because of its dense sensory innervation, including nociceptive fibres, the TLF may play an important role in lower back pain. Most of the myofascial pain may come from the superficial layer. This suggests that it may be most effective to work more superficially, stimulating proprioceptive nerve endings and reaching to the nociceptor. For many years Robert taught his students to work deeper for more profound change, but now based on this new finding, he often works more superficially to be more effective.
Figure 2. The distribution of CGRP and Substance P (SP)-immunoreactive nerve fibers in the Thoracolumbar Fascia (redrawn from Tesarz et al., 2011).
(a) Mean nerve fibre length of CGRP and SP. Almost all fibres were found in the outer layer of the fascia and the subcutaneous tissue. The middle layer was free of SP-positive fibres.
(b) Distribution of CGRP and SP-containing receptive free nerve endings expressed as percent of the total number of CGRP- or SP-containing fibers in each fascia layer. SP-containing free nerve endings were restricted to the outer layer of the thoracolumbar fascia and the subcutaneous connective tissue while CGRP-containing free nerve endings were also found in the inner layer of the thoracolumbar fascia.
In addition, Robert also suggested three areas of consideration that scientists can learn from therapists:
(1) The influence of sympathetic activation on and fascial tonicity
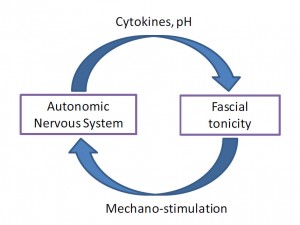
Vladimir Janda, suggested a close relationship between the autonomic nervous system (ANS) and fascial tonicity, implying that sympathetic activation may lead to an increased cellular contraction within fascial tissues. However it was not until recent findings that suggest that sympathetic activation induces an increased TGF-β1 expression; and- since this cytokine is known as the most potent stimulator of myofibroblasts contraction- that this may also lead towards an increased fascial contractility.
Figure 3 illustrates a possible two-way interaction between ANS activation and fascial tonicity. Besides the influence of the ANS on cellular contractility in fascia, this diagram also emphasises the potential influence of therapeutic fascial stimulation on ANS tuning. Stimulation of non-nociceptive mechanosensory free nerve endings can influence ANS tuning. In addition, stimulation of Ruffini corpuscles- which are reportedly particularly sensitive to slow shear application – tends to inhibit sympathetic activation.
Figure 3. Proposed interaction between the autonomic nervous system and fascial tonicity. Sympathetic activation tends to activate TGF-β1 expression (as well as probably other cytokines) in the body, which has a stimulatory effect on myofibroblast contraction, thereby leading to an increase of fascial stiffness. In addition, shifts in the autonomic nervous system state can induce changes in pH, which affects myofibroblast contraction as well. Skilful therapeutic stimulation of mechanoreceptors in fascia – particularly of Ruffini or free nerve endings – can induce changes in the autonomic nervous system (From Schelip et al. 2012).
(2) Rhythmic oscillations of fascial tissues
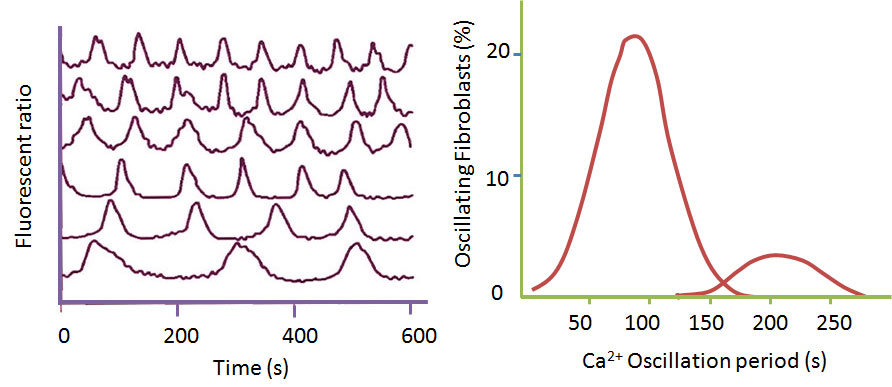
When connective tissue cells were put together in a cell culture medium with a collagen grid, they tend to show periodic oscillations. In particular, it has been shown that they expressed rhythmic calcium oscillations which were accompanied by contractions of the cells. A study by Follonier et al. (2010) demonstrated that myofibroblasts tend to oscillate in synchronicity when they were placed in a close physical contact with each other (Fig. 4). TThe observed oscillations had a mean period length of 100 second. It is an intriguing question whether this very slow rhythm observed in these cell cultures – with one cycle taking more than one and a half minutes- could be related to the so-called “long tide” oscillations in biodynamic craniosacral therapy. The so-called “breath of life” has a reported period length of 100 seconds. This needs to be tested in real-world whether myofibroblasts can express this behaviour, and related to the “breath of life”. It could of course also be just a palpatory illusion of the therapist.
Figure 4. Myofibroblasts expressed rhythmic calcium oscillations. The graph on the left showed recording of fluorescence activity of five individual cells, which were previously stained with Flura-2. The analysis revealed a common peak around 99 ± 32 seconds of the cells, as well as a second maximum of 221 ± 21 s. Based on Follonier et al. (201 0).
(3) Scientists should collaborate more following the network properties of the connective tissues
Competition in the scientific world is very strong, researchers compete to publish first, therefore, their findings or data are usually not shared and kept at secret. This is also instigated by competition for funding. Scientists should be more open to their work and collaborate more, without the fear of other people trying to steal their ideas. They should imitate the network tissues they are working on by forming a network of exchange of information.
References
Follonier, C.L., Buscemi, L.,Godbout, C., et al., 20 I 0.A new lock step mechanism of matrix remodeling based on subcellular contractile events. J. Cell Sci. 123, 1751-1760.
Schleip R, Duerselen L, Vleeming A, Naylor IL, Lehmann-Horn F, Zorn A, Jaeger H, Klingler W. Strain hardening of fascia: static stretching of dense fibrous connective tissues can induce a temporary stiffness increase accompanied by enhanced matrix hydration. J Bodyw Mov Ther. 2012 Jan;16(1):94-100. doi: 10.1016/j.jbmt.2011.09.003.
Tesarz J, Hoheisel U, Wiedenhöfer B, Mense S. Sensory innervation of the thoracolumbar fascia in rats and humans. Neuroscience. 2011 Oct 27;194:302-8. doi: 10.1016/j.neuroscience.