An Interview with Antonio Stecco
Dr. Antonio Stecco is a graduate in Medicine and Surgery, and specialized in Physics Medicine and Rehabilitation at the University of Padua, Italy. His scientific and clinical interests are anatomy of the fascia corporis via dissections and histological studies, including immunohistochemical and molecular biology; study and clinical application of hyaluronic acid; and myofascial syndrome. Following the techniques developed by his father, Luigi Stecco, PT, Dr. Stecco co-authored with his sister, Carla Stecco, MD Fascial Manipulation for Musculoskeletal Pain (Piccin, 2004).
Dr. Stecco was recently elected Assistant-President in the Cabinet of the International Society of Physical Medicine and Rehabilitation. He is also the author of 20 articles in journals, all relating to the category of disciplinary scientific sector MED/34, presentation at international conferences, including one Best Poster Award and three chapters in English textbooks.
Can you tell us a bit about your work.
I am a physiatrist and have been working more than 10 years in the department Human Anatomy and Physiology in University of Padova, Italy. My work tries to understand the anatomy and morphology of fascia, particularly the relationship between fascia and muscle. With this fundamental research and discoveries, we are able to find out fascia involved in musculoskeletal disorder and pain, and also able to explain neuropathic pain, or what is usually called myofascial pain.
What is the relationship between fascia and pain?
Myofascial pain syndrome (MPS) is usually described as symptoms on the muscle, sensory, motor, and autonomic nervous system caused by stimulation of myofascial trigger points. Its cause is still a mystery, and the role of fascia in this syndrome has often been neglected.
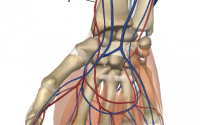
Now let us look into the anatomy of fascia first. The term deep fascia, we intend any dense fibrous sheath that interpenetrates and surrounds the muscles, bones, nerves, and blood vessels of the body, binding all these structures together into a firm compact mass. Over bones, it is called periosteum, around tendons, it forms the paratendon, around vessels and nerves, it forms the neurovascular sheath. Around joints, it strengthens the capsules and ligaments.
Deep fascia (such as fascia lata, brachial fascia, crural fascia) is not a single structure, but a multilayer structure composed of 2 to 3 layers of dense connective tissue (collagen type 1, 3, elastin fibres), and several layers of loose connective tissue (adipose tissue, GAG, and HA). The dense connective tissue has a function to transmit force, proximally to distally and vice versa, and to help the coordination of muscles. Now, we know that about 30% of the muscle insertions are not in the tendon, but in the deep fascia. All of these fascial insertions provide an excellent illustration of how the thickness and strength of fasciae is a precise mirror of the forces generated by muscular action. When these muscles contract, not only do the bones move, they also stretch the deep fascia.
Meanwhile the loose connective tissue is structured so that they are independent of each other, each layer have a particular direction of collagen fibre that follow the muscle fibre. It allows gliding between each layer and between the layer and the muscle.
Deep fascia is also innervated with many mechanoreceptors (such as Ruffini, Pacini, free ending nerves). Research from Heidelberg led by Siegfried Mense also described that fascia is innervated with nociceptors. Fascia is therefore important in proprioception and pain generation. It is possible that the viscoelasticity of fascia can modify activation of the nervous receptors within fascia
For example, if the viscosity of the connective tissue change, the gliding between the layers of fascia can be affected (decreased). If a decrease between layers of the deep fascia, they will start to experience stiffness. This will cause hyperactivation or irritation of the mechanoreceptors, free ending nerves, and eventually pain. This pain experience, however, will not show up in any x-ray or MRI because it is not a morphological change that caused the pain, but the alteration of the viscosity of connective tissues.
In an experiment using ultrasound, we showed that neck pain is proportional to the fascial thickness of the sternal ending of the sternocleidomastoid and medial scalene muscles. After FM treatment, the results showed a significant decrease in loose connective tissue thickness.
There are now different studies using an instrument that can stretch the fascia in the lab. Initially the fascia from a cadaver is very stiff, but after several stretching cycles the stiffness begins to decrease. This is like a ‘warm up’ exercise. In human, the opposite could happen. In overuse or repetitive use syndrome, isometric contraction for a long time can increase the viscosity of the HA, causing an increase stiffness.
What is the Role of Hyaluronic Acid (HA) in pain generation?
HA is a large, remarkably simple, straight chain carbohydrate polymer of the extracellular matrix (ECM). This is in marked contrast with all other GAGs that are attached to core proteins. High molecular size HA in the body acts as a hydrating, space filling polymer. We have confirmed that HA is located in considerable amounts at the interface between deep fascia and the surface of muscle. This provides a lubricant for the fascia to glide over neighbouring muscle.
The viscoelasticity of the fascial tissue and associated HA shapes the dynamic response of the mechanoreceptors. The normal sliding lubricating function of HA can decrease with increased viscosity. When the HA becomes adhesive rather than lubricating, the distribution of lines of force within the fascia become altered. With increase viscosity, the receptors within the fascia can send a pain message even when it is stretched within the physiological range.
How does manual therapy able to help?
Therefore an important component of manual therapy is to reverse these changes in HA. From clinical and lab experiments, we demonstrate that with deep pressure, friction and gliding, we are able to create an increase in temperature in the deep fascia. That’s why in Fascial Manipulation® (FM®) we keep the pressure and create a gliding in a particular spot because it increases the temperature. In the lab we showed that when we reach over 40 degree Celsius, we are able to break down the chains by inter- and intra-molecular water bonds of HA, and thus can decrease viscosity. The decrease of the viscosity enables restoration of normal gliding and normalizes the activation of the mechano-receptors in that area. The HA fragmentation reactions also promote inflammation that help to restore the normal physiology of the area.
Our idea in Fascial Manipulation® is that with deep pressure, we warm up the area, catalyse inflammatory reaction, restore the fluidity (from gel to sol) of HA, and thus restore normal gliding. The real efficacy of the manipulation of deep tissue lies in its role as a catalyst for resolving the inflammatory reaction.
How does fascia relate to proprioception?
The perspective of the body in space now it is a very popular concept, but twenty years ago when we said that fascia is an organ for proprioception people are surprised and find it difficult to digest. The fascia is innervated, surrounds the muscle and it can “feel” the elongation and changes in the muscles. When we use our muscles, whether moving, elongation, contraction, we pull through the myofascial insertion, a particular area of the fascia. Because fascia is innervated, the mechanoreceptors in the area will be stretched, and activated. The CNS will have a “map” of the mechanorecteors throughout the body. So if a particular area is activated, the CNS will know that a particular region of the body is affected or moving in space. Muscles, fascia, nerves, CNS work together to perceive the movement in space.
Can you tell us about FM for Internal Dysfunctions
The Level III of Fascial Manipulation is indicated for visceral pain and symptoms as constipation, dysmenorrhea, reflex and all the other symptoms of the organs when the imaging do not show any morphological alteration. FM for internal dysfunctions evaluate also the alteration of the superficial fascia as oedema, alteration of the superficial vein system, skin alteration etc. with a different modality of treatment and a new type of manuality.
The points that we treat are almost the same (we have added only some points), but the combination and the modality of the approach is completely different. This allow the therapist to asses and treat symptoms that, most of the time, were difficult to interpret. We teach how the manipulation of the container (fasciae of the trunk) and extremities restore the normal tension of the fascia restoration the correct motility and function of the organ. Our approach is related at the tensile structure of our body that allow us to work out the body to effect inside the body.
What is your current work?
Now, we are doing research in anatomy and physiology of fascial, with collaborations of University of Padova, Rehab. Centre in Sao Paulo and other places. I am using ultrasound techniques to objectively show the effect of treatment on the changes in fascia and improvement of the fascia gliding.
I am also travelling all over the world (this year I have travelled to New York, Las Vegas, Houston, Washington DC, Los Angeles, Manila, Hong Kong, Beijing, Dubai, Tokyo and Europe) teaching Fascial Manipulation®. The FM book is now translated in Japanese, Korean, Chinese, Portuguese, English, Polish, France, Italian, Spanish and German. We want to popularise FM for everybody because it is a relatively cheap, fast, and effective method to treat musculoskeletal pain. The government in Israel now recognised FM as one of the 3 best manual therapies. In the US, private health insurance looks for treatments that can show improvement after three treatments, and FM is a perfect method for this. The treatment is easy to teach, even to Medical Doctors, and they found it is easy to restore the function and pain.