Effectiveness of various methods of manual scar therapy
Scars can form as a result of various factors such as mechanical damages, burns, surgeries, and long-lasting skin diseases, and they can affect most people. Scars can be normal or pathological, with factors such as age, anatomic location, race, and type of trauma increasing the risk of pathological scarring. Pathologic scar formation can lead to low tensile strength, pigment alterations, increased tension texture, and sensation irregularities.
The formation of excessive scar tissue can lead to changes in cosmetic appearance, continuing pain, and loss of movement, which can significantly affect a person’s quality of life and psychological recovery after injury.
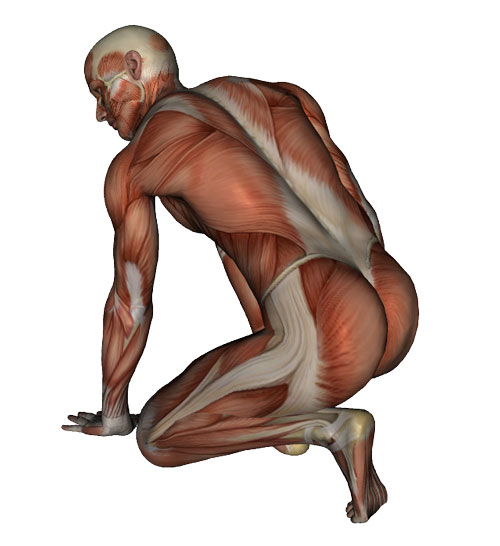
Physical scar management includes different treatment methods such as manual therapy, appropriate pressure, taping, cryotherapy, dermabrasion, radiation, laser therapy, pharmacological methods, and surgical techniques.
Scar tissue therapy aims at reducing pain and functional limitations, improving pliability, reducing hyperpigmentation, pruritus, fascial adhesions, to reduce scar thickness, and smooth surface area. Scar massage is one such therapy
A study from Poland involved eleven female volunteers with postoperative scars, aged between 27 and 39 years, who had not received any scar therapy. The patients received a standardized treatment protocol that included manual scar manipulation, massage, cupping, dry needling, and taping. Objective and subjective evaluations of the scars were carried out using clinical photography, measurement of skin parameters, high-frequency ultrasound, and the Patient and Observer Scar Assessment Scale (POSAS).
The study shows that manual scar therapy can improve the appearance of scars by making them paler, flatter, and more regular. High-frequency ultrasounds (HFUS) were used to assess the influence of scar manual therapy on scar height and their structure, and differences in scar structure were observed with statistical significance. The study also found differences in skin parameters, including hydration, transepidermal water loss (TEWL), stretchability, and erythema level. Patient self-assessment using the patient component of the POSAS showed statistically significant improvements in pain, pruritus, color, stiffness, regularity, vascularization, and elasticity after therapy.
The study concluded that manual scar tissue therapy involving various methods and techniques need to be adapted to each patient individually. The therapy, which includes scar massage, soft tissue manipulation, cupping, dry needling, and taping, has shown significant positive effects on pain, pigmentation, pliability, pruritus, surface area, and scar thickness. However, further studies are needed to determine the most effective manual therapy strategy and establish a protocol of effective intervention.