Effects of myofascial release of the diaphragm on acid reflux condition
Gastroesophageal reflux disease (GERD), also known as acid reflux or heartburn, is a digestive disorder, where stomach acid frequently flows back into the oesophagus, the tube that connects the mouth and stomach. It causes discomfort and complications. The prevalence is around 20% in the western world. Current standard medical treatment includes the administration of proton pump inhibitors drug (PPIs). Long-term consumption of PPIs can have negative side effects.
Studies have demonstrated that performing periodic respiratory exercises aimed at strengthening the crura of the diaphragm (CD) can be an effective non-pharmacological treatment that can help patients with GERD. The idea of exercising the diaphragm is that the CD is a key component of the anti-reflux barrier because it functions as an extrinsic esophagogastric junction sphincter.
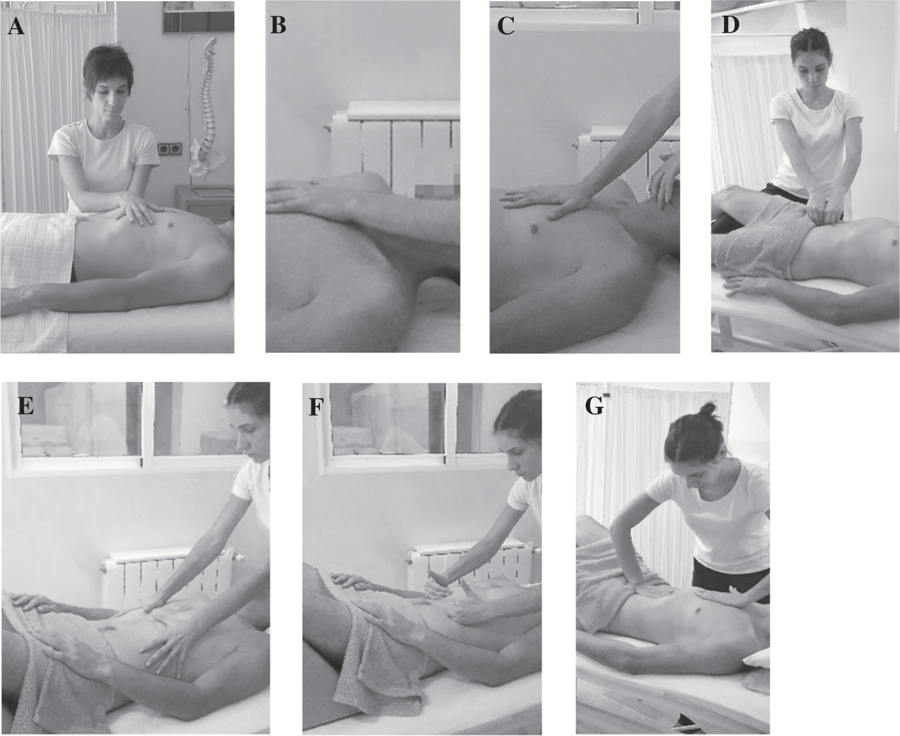
A study from Spain looked at the effect of myofascial release (MFR) of the diaphragm protocol on patients with acid reflux condition. The study involved 30 patients with GERD who were randomised into an MFR group or a sham group. The MFR group received a myofascial release of the diaphragm protocol consisting of four sessions, each one lasting 25 minutes (twice a week for two weeks). The sham group received the same type of contact treatment, following the respiratory movements but without applying any fascial stimulus or pressure, on the same schedule as the MFR group.
The effect was measured by changes in symptomatology and quality of life using the Reflux Disease Questionnaire and the Gastrointestinal Quality of Life Index. They also recorded the consumption of PPIs measured as the milligrams of drug intake over the 7 days before each assessment. All variables were assessed at baseline, one week, and 4 weeks after the end of the treatment.
Results showed that at week 4, patients receiving MFR showed significant improvements in symptomatology, gastrointestinal quality of life, and decrease in PPIs use when compared to the sham group.
The authors hypothesised that MFR improves diaphragmatic mobility and visceral fascial mobility. Considering that optimal phrenoesophageal membrane slip is necessary for correct anti-reflux barrier function, applying MFR treatment may improve the function of the crura of the diaphragm–oesophagus sliding component.
Nevertheless, the authors stated limitations of the study:
This was only a small preliminary trial, and the study did not assess whether the diaphragm was blocking the esophagus. They also note that the practitioner responds to the needs of each person’s body, every therapy session is different.
These preliminary findings indicate that the application of the MFR protocol decreased the symptoms and PPIs usage and increased the quality of life of patients with non-erosive GERD up to four weeks after the end of the treatment.
Myofascial release protocol for the intervention group. (A) Diaphragmatic transverse plane. (B) Anteroposterior equilibrium technique. (C) Supra and infrahyoid fascial induction. (D) Psoas fascial induction. (E) Diaphragm stretching technique: first step. (F) Diaphragm stretching technique: second step. (G) Phrenic centre inhibition. (From I. Martínez-Hurtado et al. 2019)