Fascia therapy decreases unbound water
The capacity of fascia to soften or harden in response to mechanical stimuli has attracted new research interest. For example, isometric stretching could alter the water content of fascia and can have an impact on the viscoelasticity of tissues. It was hypothesised that a healthy ground substance in fascia contains abundant proportion of water “bound” to glycosaminoglycan (GAG). GAG is a component of the ground substance of the extracellular matrix, which functions to maintain tissue hydration. Local inflammation is assumed to reduce this bound water. Fascia therapy was considered to squeeze out the stagnant water so that the new water can flush into tissues.
Experiment has shown that an increase in hyaluronic acid concentration, the chief component of the GAG, can trigger a self-aggregation, which increased the viscosity in the extracellular matrix. This alteration can affect nociceptors by decreasing their pain sensitivity threshold. This means that pain signals can easily be generated from abnormal peripheral tissues (for example, stiff fascia) and transmitted, by the dorsal horn pain transmission neurons, to the brain.
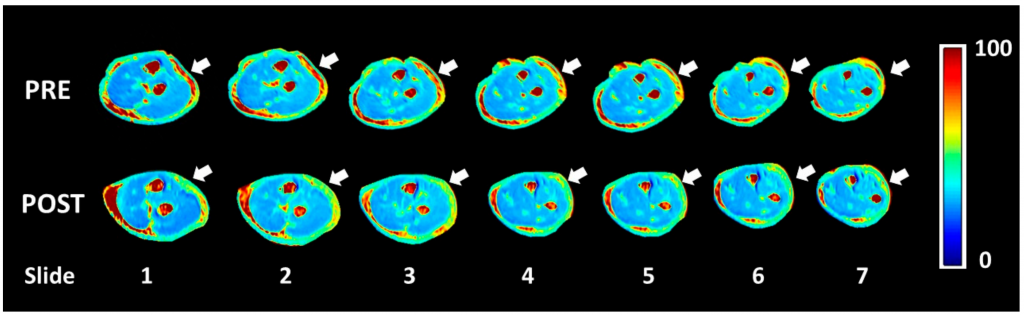
A new imaging technique called T1ρ mapping that used magnetic resonance has been recently applied to picture water-bounded content in muscles. T1ρ mapping can “see” chemical exchange between extracellular water (unbound water) and macromolecules (bound water). This method has been used to quantify proteoglycan content in cartilage, muscle, and intervertebral discs. It is now used for indirect quantification of glycosaminoglycan (GAG) content in tissues.
The study was published in Environmental Research and Public Health.
Five patients presenting chronic elbow pain (>3 months), with age between 30 and 70 years old were recruited. Their forearms were imaged using the T1 mapping before and after a series of Fascial Manipulation® (FM) treatments (three sessions of FM, once a week for 40 min each). The imaging focussed on antebrachial fascia (deep fascia).
The results showed a statistically significant difference between bound and unbound water concentration before and after FM treatment. The application of manual therapy decreased the level of unbound water inside the deep fascia only in the most chronic patients.
The authors hypothesized that this phenomenon could explain the change in tissue viscosity felt by manual therapists. The decrease of pain symptoms could be due to the restoration of the normal property of the loose connective tissue.
Being able to identify an altered deep fascial area may better guide therapies, contributing to a more nuanced view of the mechanisms of pain.
Pre- and post-T1ρ-mapping of brachial fascia. The white arrows show the areas that were considered the most symptomatic from the patient. It can be seen a change from red (unbound water) in the pre-treatment to green-blue (bound water that works as a lubricant) in post-treatment. From Menon et al. 2020 (CCy BY) https://www.mdpi.com/1660-4601/17/3/708/htm