Fascial tissue research in sports medicine
Fascial tissues deserve more detailed attention in the field of sports medicine.
This consensus statement published in British Journal of Sport Medicine is an outcome of the Second International CONNECT Conference held at the University of Ulm, Germany, on 16–19 March 2017. The statement was authored by 12 international scientists include Martina Zügel, Jan Wilk, Tom Findley, Andry Vleeming, Robert Schleip, Paul Hodges and others who aimed at fostering scientific progress towards a better understanding and treatment of fascial tissues in sports medicine.
Injuries to a variety of fascial tissues cause a significant loss of performance in sports and have a potential role in the development and perpetuation of musculoskeletal disorders, including lower back pain. A major goal of clinicians is to return athletes and patients to activity, training and competition after injury. Thus, a better understanding of their adaptation dynamics to mechanical loading as well as to biochemical conditions promises valuable improvements in terms of injury prevention, athletic performance and sports-related rehabilitation.
The consensus statement reflects the state of knowledge regarding the role of fascial tissues in the discipline of sports medicine.
Definition
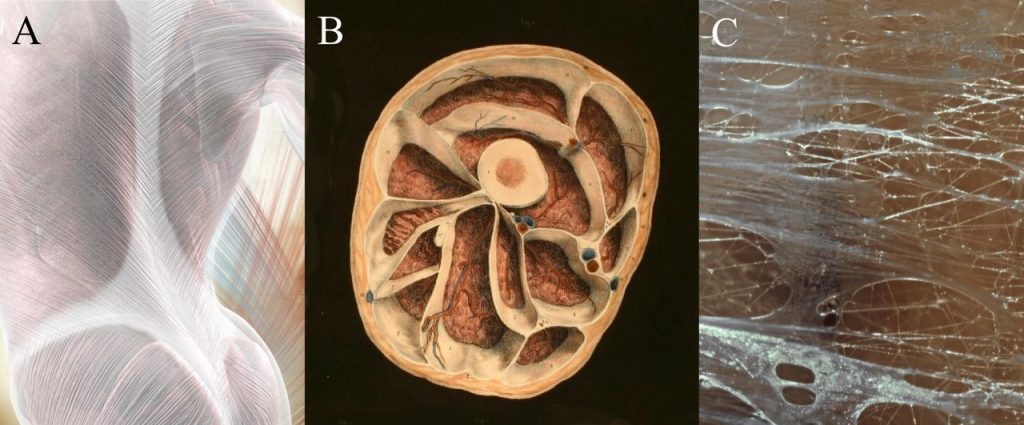
The fascial system includes adipose tissue, adventitia, neurovascular sheaths, aponeuroses, deep and superficial fasciae, dermis, epineurium, joint capsules, ligaments, membranes, meninges, myofascial expansions, periostea, retinacula, septa, tendons (including endotendon/ peritendon/ epitendon/ paratendon), visceral fasciae, and all the intramuscular and intermuscular connective tissues, including endomysium/perimysium/epimysium.
Molecular adaptation of fascial tissues
Molecular crosstalk between extracellular matrix (ECM) molecules and cellular components is an important determinant of fascial tissue physiology and pathophysiology.
Small functional and structural alterations in the ECM result in complex cellular adaptation processes and, vice versa, changes in cell function and structure leading to ECM adaptation. Therefore, fascial tissue homeostasis is the result of a complex interplay and dynamic crosstalk between cellular components and the ECM. Under dynamic conditions such as growth and regeneration, strong alterations of the local ECM microenvironments are necessary to allow cellular adaptation and rebuilding of fascial tissues. ECM is affected by ageing, sex hormones and inflammation.
Myofascial force transmission
Experiments in animals and imaging studies in humans have shown that intermuscular and extramuscular fascial tissues also provide a pathway for force transmission, which in part, is depenedent on the mechanical properties of myofascial tissue linkages. Initial in vivo evidence points towards a significant role of myofascial force transmission for the locomotor system. It has also been shown the existence of (1) remote exercise effects and (2) non-local symptom manifestations in musculoskeletal disorders, both of which might be of relevance in athletic and therapeutic settings.
Injury of fascial tissues: cellular and mechanical responses to damage
Excessive or prolonged loading or direct trauma to fascial tissues initiates micro and macro changes necessary for tissue repair. These effects may also contribute to pathological changes that modify tissue function and mechanics, leading to compromised function of the healthy tissue. Exercise, physical modalities and pharmacological interventions have all been shown to reduce the inflammatory processes associated with fascial tissue injury and fibrosis.
Mechanobiology of fascial tissues: effects of exercise and disuse
Human tendons respond to the application of chronic overloading by increasing their stiffness and to chronic unloading by decreasing their stiffness. The mechanisms underpinning these adaptations include changes in tendon size and changes in Young’s modulus. Tendon adaptations occur quickly, within weeks of mechanical loading/unloading application. Importantly, however, some studies report adaptations in tendon size but not tendon material, and others in tendon material but not size, while some report adaptations in both tendon size and material
Interventions for fascial tissue pathologies in sports medicine
Fascial tissue dysfunction in the field of sports medicine is rarely treated surgically. Anti-inflammatory drugs are used for sports-related overuse pathologies; however, they may impair regeneration and diminish tissue adaptation.
Foam rolling seems to improve short-term flexibility and recovery from muscle soreness and decrease latent trigger point sensitivity. Nevertheless, the physiological mechanisms of these reported effects remain unclear, although initial evidence suggests increases in arterial perfusion, enhanced fascial layer sliding and modified corticospinal excitability following treatment. Manual therapies, such as massage, osteopathy or Rolfing, are frequently used to improve fascial tissue regeneration or athletic performance, although their efficacy still remains to be validated.
The authors concluded that advancing this field will require a coordinated effort of researchers and clinicians combining mechanobiology, exercise physiology and improved assessment technologies.
Components of the fascial system. The fascial system includes large aponeuroses like the first layer of the thoracolumbar fascia (A), but also a myriad of enveloping containers around and within skeletal muscles (B) and most other organs of the body. The internal structure of fascial tissues is dominated by collagen fibres which are embedded in a semiliquid ground substance (C). Figure from Zügel et al. (2018) CC-BY-NC.