Low back pain is a Global Problem: Time to Consider Massage and Exercise as Effective Treatments
The Lancet medical journal recently published three papers on Low Back Pain which asserted that low back pain has increased dramatically in recent years and is now the leading cause of disability globally. The review found that most medical treatments for low back pain rely heavily on scans, surgeries and opioids prescriptions that are mostly ineffective and can be harmful. The authors called for more effective treatments through self-management and less-invasive physical and psychological therapies, including complementary therapies such as massage.
Professor Rachelle Buchbinder from Monash University in Australia, the lead author of one of the papers, said that a radical shift in thinking was required. The burden from low back pain has reached a tipping point where the condition is growing rapidly, is poorly understood and is being mismanaged medically — at cost both to the patient and to the healthcare system.
In the first paper, Jan Harvigsen from Denmark and colleagues highlight that the leading cause of disability worldwide and estimated that the disability caused by low back pain has increased by 54% between 1990 and 2015, mainly because of population increase and ageing, with the biggest increase seen in low-income and middle-income countries.
Most of the low back pain is idiopathic. People with physically demanding jobs, physical and mental comorbidities, smokers, and obese individuals are at greatest risk of reporting low back pain. Disabling low back pain is over-represented among people with low socioeconomic status.
Most people with new episodes of low back pain recover quickly; however, recurrence is common and in a small proportion of people, low back pain becomes persistent and disabling. Initial high pain intensity, psychological distress, and accompanying pain at multiple body sites increases the risk of persistent disabling low back pain. Increasing evidence shows that central pain-modulating mechanisms and pain cognitions have important roles in the development of persistent disabling low back pain.
Cost, health-care use, and disability from low back pain vary substantially between countries and are influenced by local culture and social systems, as well as by beliefs about cause and effect. Disability and costs attributed to low back pain are projected to increase in coming decades, in particular in low-income and middle-income countries, where health and other systems are often fragile and not equipped to cope with this growing burden.
In the “Prevention and treatment of low back pain” article, the authors recommended:
- Self-management, physical and psychological therapies, and some forms of complementary medicine, and place less emphasis on pharmacological and surgical treatments; routine use of imaging and investigations is not recommended.
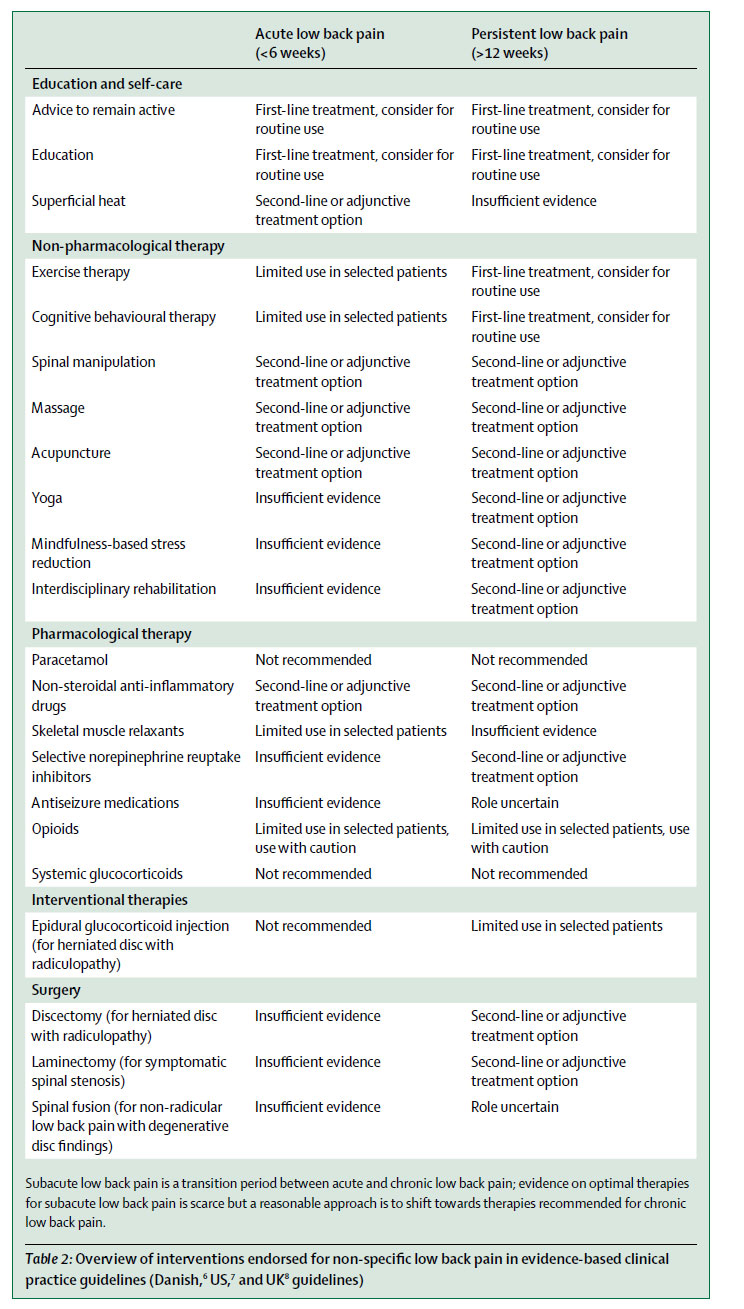
The table below from the paper lists some of the recommended treatments. The first-line of treatment is education and self-care. While spinal manipulation, massage and acupuncture were listed as second-line or adjunctive treatment option for acute and chronic low back pain.
- For prevention, little research exists, with the only known effective interventions for secondary prevention being exercise combined with education, and exercise alone
- Non-evidence-based practice common problems are presentations to emergency departments and liberal use of imaging, opioids, spinal injections, and surgery
- Promising solutions include focused implementation of best practice, the redesign of clinical pathways, integrated health and occupational care, changes to payment systems and legislation, and public health and prevention strategies
The last paper is a call for action by Buchbinder and colleagues who argue that persistence of disability associated with low back pain needs to be recognised and that it cannot be separated from social and economic factors and personal and cultural beliefs about back pain. They urge global organisations such as WHO to take action to try to reduce the increasing and costly effects of disabling low back pain. A major challenge will be to stop the use of harmful practices while ensuring access to effective and affordable health care for people with low back pain.
See Also: