Modelled Myofascial Release Enhances Wound Healing in Bioengineered Tendons through Fibroblast Proliferation and Collagen Remodeling
MFR reduces swelling and inflammation, attenuates myofascial pain, enhances wound healing. The mechanism on wound healing and regulation of the local inflammatory response attributed to fibroblasts, the primary cell type in connective tissue. Fibroblasts respond to mechanical stimuli leading to gene expression modifications and therefore are considered a target for MFR treatment.
Researchers from the Department of Basic Medical Sciences at University of Arizona studied the mechanisms of action of myofascial release (MFR) on wound. To study the fundamental of the action, the researchers used bioengineered human tissue. The study was published in Journal of Manipulative and Physiological Therapeutics.
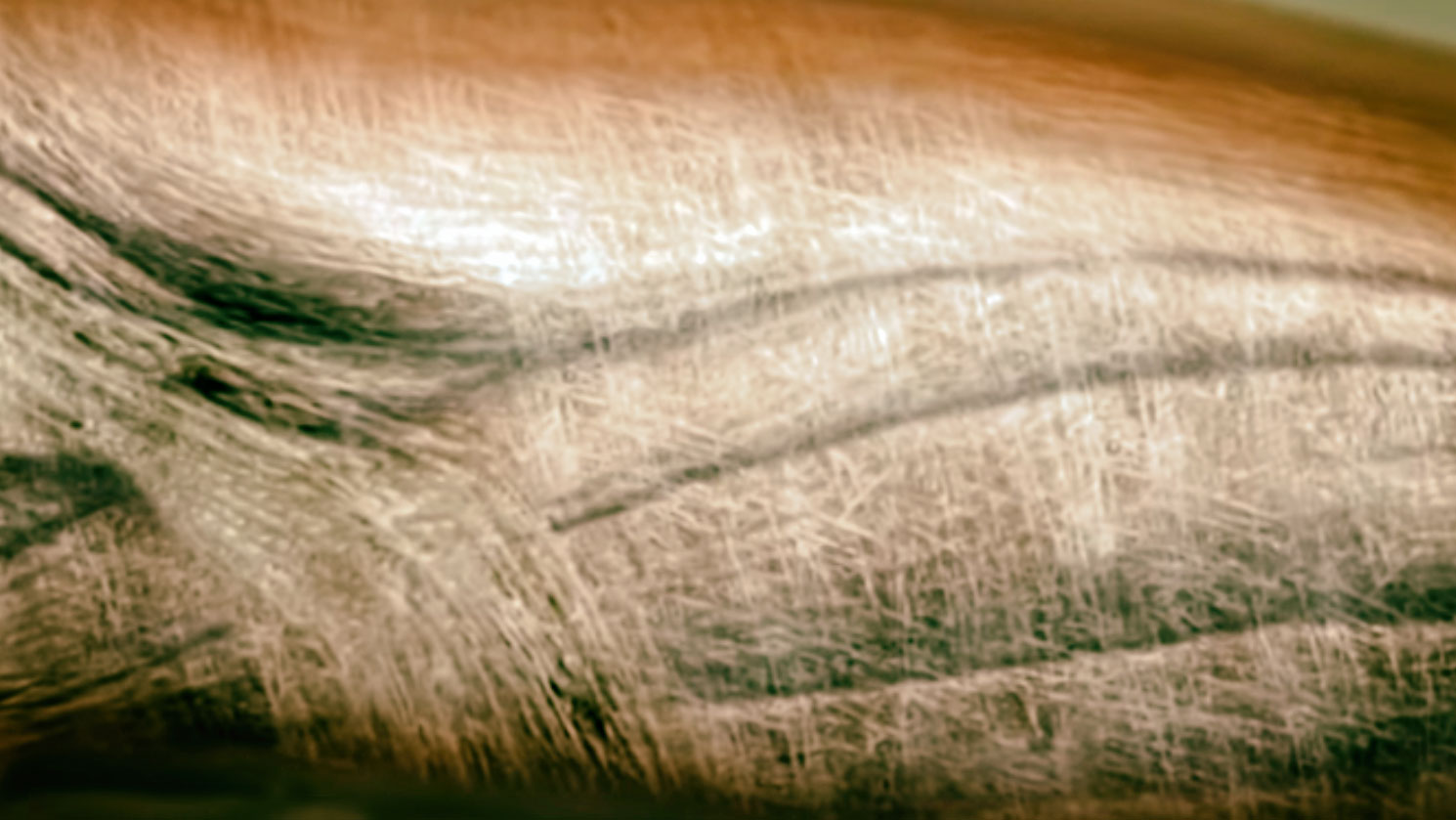
The researchers created bioengineered tendons which were cultured on a deformable matrix. The tendon was wounded using a steel cutting tip. MFR was mimicked on the wounded tissue using a mechanical strain model. Strain was slowly applied to elongate the tissue to 2.5% of its resting length per second to reach 103% of its initial resting length. The tissue was then held at 3% elongation for 5 minutes. The strain was then slowly released back to baseline at a rate.
Imaging and measurements of the width and wound size were performed daily, and the average tissue width of the entire bioengineered tendon was measured and wound size and major and minor axes of the elliptical wound were additionally measured.
The results showed that the modelled MFR treatment significantly reduced the wound size and increased both collagen density and cell deposition at the wound site. All measures of wound healing improvements required the presence of proliferating fibroblasts.
The authors concluded that MFR results in improved wound healing due to increased fibroblast deposition and collagen density within and adjacent to the wound area. Such effects are impaired in injured tissues, wound healing impairment may be correlated to loss of human fibroblast collagen secretion and integration into the extracellular matrix.
If clinically translatable, the results support a mechanism by which MFR improves patient wound healing.