Reimagining Human Anatomy: A New Framework Centered on the Fascial System
Ttraditional anatomical models tpredominantly influenced by the work of Andreas Vesalius in the 16th century—established a duality between bones and muscles, where bones are seen as rigid supports and muscles as the primary agents of movement. This musculoskeletal framework, often referred to as “Vesalius Anatomy Mapping” (VAM), has become deeply embedded in the medical and scientific communities. While useful in many respects, the VAM model tends to oversimplify the complexity of the human body by isolating each component and portraying it as a mechanical system akin to a machine, where individual parts operate independently.
Authors Graham Scarr, Leonid Bylum, Stephen Levin and Susan Lowell de Solorzano proposed a new framework of anayomy in Medical Hypotheses journal.
The Cartographic Paradox in Anatomy
The critique is framed around what is referred to as the “cartographic paradox.” This paradox is based on the concept that anatomical descriptions are analogous to geographical maps—they serve as simplified, schematic representations of a much more complex reality. Just as a map highlights only key features and relationships while omitting finer details, anatomical models like VAM offer selective views of human structure and function.
Monmonier’s observation, “To avoid hiding critical information in a fog of detail, the map must offer a selective, incomplete view of reality,” encapsulates this issue. Applying this notion to anatomy, the VAM framework has led to a biased emphasis on bones and muscles as the principal actors in movement and stability, while other critical tissues, such as fascia, have been relegated to secondary roles.
The Legacy of Vesalius and the Musculoskeletal Duality
The origins of this oversimplified view trace back to the revolutionary work of Andreas Vesalius. His 1543 book, De humani corporis fabrica (On the Fabric of the Human Body), was groundbreaking for its time. Vesalius’ anatomical drawings emphasized a clear distinction between the bones and muscles, positioning them as separate entities with specific roles. Bones were portrayed as the rigid scaffolding of the body, while muscles were the active movers attached to this framework.
This structural depiction, while transformative, reinforced the idea of bones and muscles as mechanistic components, akin to beams and pulleys in engineering. Such a perspective was appealing and computationally efficient, allowing researchers to model movement through simple mechanical equations. However, it also created an inherent limitation by omitting the nuanced role of connective tissues, such as fascia, which do not fit neatly into this binary categorization. Fascia, for instance, was historically dismissed as mere “packing material” with little functional significance.
The Lever Problem and the Instability of the Musculoskeletal Model
Viewing bones as rigid structures and muscles as levers that move these structures creates a problem: such a system cannot passively stabilize itself when faced with unexpected forces or perturbations. Instead, it relies on reactive muscle contractions, mediated through neural control, to maintain balance and coordination. This reliance on muscular reflexes to provide stability introduces a time-delay, as even the fastest reflexes are not instantaneous. During sudden or abrupt changes in force dynamics, this latency can lead to transient peak stress concentrations that the body cannot adequately manage. Over time, these mechanical instabilities may contribute to material fatigue, tissue damage, and a greater risk of injury, particularly when forces exceed the capacity of muscles to respond.
The standard biomechanical models often focus on steady-state conditions, assuming that forces and movements are smooth and predictable. This approach, however, overlooks the critical role of transient dynamics—the abrupt changes in force that can have a significant impact on tissue integrity. Recent studies have shown that the rate of change of force (referred to as “jerk” in physics) and even higher-order derivatives such as snap and crackle play a crucial role in determining tissue responses. When these factors are not accounted for, the resulting models can oversimplify real-world biomechanics, leading to a distorted understanding of how the body operates under dynamic conditions.
Moving Beyond Musculoskeletal Models: Introducing MMAM
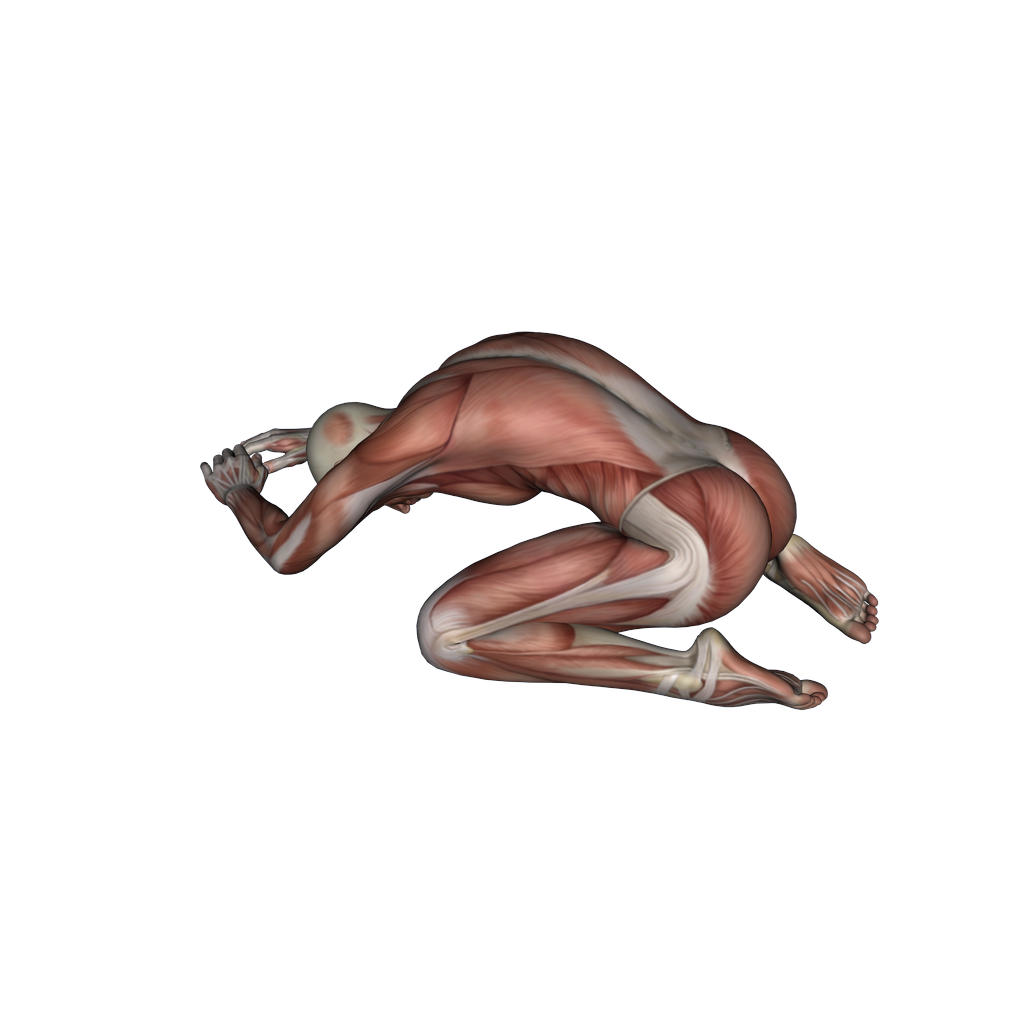
To address these limitations, tan alternative approach is proposed: the Modernized Malpighi Anatomical Mapping (MMAM) framework. Named after Marcello Malpighi, who first described the cellular structure of tissues in the 17th century, this model reconceptualizes anatomy by positioning the fascial system—not bones or muscles—as the primary structural network. The MMAM framework views the body as a hierarchical system of interconnected fascial compartments, each functioning as a distinct yet integrated unit within the broader architectural framework. This approach shifts the focus from isolated musculoskeletal components to a comprehensive view of connective tissue dynamics.
The Role of Fascia in the MMAM Framework
Fascia is no longer considered a passive, secondary structure but a dynamic, tensioned network that supports, connects, and facilitates movement across all tissues and organs. The MMAM framework proposes that fascia acts as a globally tensioned network that maintains structural integrity and distributes forces throughout the body. From the cellular level to large-scale anatomical regions, fascia and its extensions form a continuous system that encapsulates and interweaves between muscles, bones, organs, and nerves. This interconnectedness allows the fascial system to transmit mechanical forces and coordinate movement in a way that the traditional musculoskeletal paradigm cannot explain.
The MMAM model has significant implications for how we understand bodily stability and movement. It proposes that bones, muscles, and organs are not discrete elements but rather specialized fascial compartments that have adapted to perform specific roles within the fascial matrix. For example, bones, traditionally seen as rigid supports, are reframed as highly specialized, mineralized compartments that contribute to the overall stability and elasticity of the fascial network. Similarly, muscles are reinterpreted not as isolated motors but as parenchymal structures embedded within a complex fascial hierarchy that modulates their shape, tension, and function.
Implications for Biomechanics and Medicine
Adopting the MMAM model could revolutionize the fields of biomechanics, physical therapy, and clinical medicine by shifting the focus from muscle-centric treatment approaches to a more holistic view of connective tissue health and function. It suggests that many musculoskeletal disorders, such as compartment syndromes, myalgia, and even some inflammatory diseases, may be better understood and treated by targeting fascial dysfunctions rather than solely focusing on bones and muscles. For example, conditions like fibromyalgia, traditionally viewed through the lens of muscular pain, may be reinterpreted as disorders of fascial tension and compartmental dynamics.