Structural and Functional Changes in the Neuromyofascia system During Aging
Aging is a natural process that can cause significant changes in the neuromyofascia system, including muscles, fascia, and the central and peripheral nervous systems. The structure and function of myofascial tissues will be affected. A review by Alberto Zullo and colleagues published in Frontiers in Physiology summarized the evidence about the harmful effect of aging on skeletal muscle, fascial tissue, and the nervous system.
The scientific literature demonstrates that senescence is associated with increased stiffness and reduced elasticity of fascia, as well as the loss of skeletal muscle mass, strength, and regenerative potential. The interaction between muscular and fascial structures is also weakened. As for the nervous system, aging leads to motor cortex atrophy, reduced motor cortical excitability, and plasticity, thus leading to the accumulation of denervated muscle fibres.
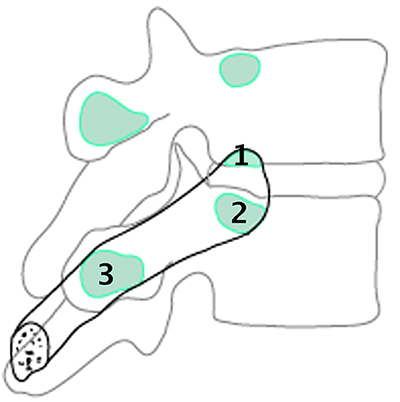
The close interaction between muscular and fascial structures and the physical continuity of connective tissue along the myofascial chain could weaken with age, thus reducing the magnitude of mechanical force transmission. Fascial tissue can densify and develop fibrosis with age, thus reducing muscular force production and joint range of motion. Decreased physical mobility occurring in the elderly could be partially explained by increased stiffness and reduced elasticity of the extracellular matrix due to dehydration and increased collagen content. Thus, with aging, the magnitude of force generated by the neuromuscular apparatus, its transmission along the myofascial chain, joint mobility, and movement coordination could be impaired.
A key feature of aging tissue is, the so-called “inflammaging”, which describes a low-grade chronic systemic inflammation in the absence of overt infection. This “sterile” inflammation is a highly significant risk factor for morbidity and mortality in elderly people. Most of the inflammatory responses take place in the extracellular matrix, which can interact with immune cells and change their functions, thereby influencing tissue regeneration. Although early inflammation after tissue damage is essential for remodeling and adaptations, decreased inflammation seems to be associated with improved tissue regeneration and gains of muscle strength.
From the perspective of healthy aging, it is crucial to identify and hinder all the age-dependent modifications through specific strategies targeting etiologic factors, and also psycho-social issues. Tissue manipulation techniques might contribute to improving myofascial regeneration in the elderly. A study performed on people suffering from delayed-onset muscle soreness showed that the sensitivity of high-threshold mechanosensitive receptors is a predictor of pain and motor impairment. Thus, approaches modulating the activity of these receptors may be helpful for functional recovery. There is evidence that multimodal rehabilitation, including classic massage, transcutaneous electrical nerve stimulation, and ultrasound therapy improves pain and function in older women (aged >60) suffering from back pain. In summary, the authors hypothesized that the fascial tissue of older adults is susceptible to soft tissue stimuli, but its effect has to be determined.
Physical activity has also been suggested as an effective strategy for counteracting the harmful consequences of aging, given that skeletal muscle plasticity might be only partially lost in elderly individuals. However, this issue is still debated due to contradictory results. Nevertheless, the constant progress in technology and biomedical research holds great promise for fighting the burden of aging by targeted therapeutic interventions.