There is a Third Deep Layer of the Iliotibial Band
 A new research from orthopeaedic surgeons from Austria shows the existence of a deep layer of the ITB.
A new research from orthopeaedic surgeons from Austria shows the existence of a deep layer of the ITB.
Fascia Latae and Iliotibial Band (ITB)
The thigh is enveloped in a layer of fibrous tissue known as the fascia latae, which thickens in the lateral thigh and is described as the iliotibial band (ITB). The ITB is well recognized as having two layers, one superficial to the tensor fasciae latae (TFL) muscle, and the other deep to the TFL. But it is not generally known that the ITB actually has a third layer that lies deep to its other two layers. Therefore, the ITB actually has three layers: superficial, intermediate, and deep layer.
The ITB
The ITB attaches on the iliac crest and extends distally to the anterolateral side of the proximal tibia onto an attachment site known as Gerdy’s tubercle. The three layers of the ITB fuse in the region of the greater trochanter and form the proximal ITB. The superficial layer arises from the ilium superficial to the TFL, while the intermediate layer arises from the ilium slightly distal to the proximal attachment of the TFL and lies deep to the muscle. The superficial and intermediate layers of the ITB merge at the distal end of the TFL and serve as the tendon for the TFL.
The ITB is connected intimately with the TFL anteriorly and the gluteus maximus (GM) posteriorly in the region distal to the greater trochanter. The ITB is not fixed at the greater trochanter, but uses it as a diversion point.
The distal tendon of the gluteus maximus and a major portion of ITB intermingle near the gluteal tuberosity on the proximal posteromedial femur.
However, even though many studies on the ITB have been done and much is known, little information in the anatomy literature is available regarding the (third) deep layer of the ITB.
The Austrian Study
In an effort to better understand the structure of the ITB, especially its deep layer, a group of orthopaedic surgeons from Austria recently published a study. Their interest in the detailed anatomic knowledge derives from their interest in minimally invasive total hip arthroplasty surgery.
The study used ITBs from 20 human cadavers, where both hips were included resulting in 40 measurements with reference to the anterior superior iliac spine (ASIS) and the tibia. The deep layer of the ITB was exposed up to the hip joint capsule, and width and length measurements were taken. Sections of the deep layer of the iliotibial band were removed from the hips and the thickness of the sections was determined microscopically after staining.
The Deep Layer of the ITB
The deep layer is a constant structure arising from the supra-acetabular fossa between the hip capsule and the tendon of the reflected head of the rectus femoris. This deep layer merges into the ITB just distal to where the superficial and intermediate layers of the ITB fuse.
The mean maximum thickness of the deep layer was 584 μm, in other words, a millionth of a meter. Its width was found to be approximately 3 cm (3.3 ± 0.6 cm). And its mean length was found to be approximately 10 cm (10.4 ± 1.3 cm); however, unlike the superficial/intermediate aspect of the ITB whose length (50.1 ± 3.8 cm) was found to be related to the length of the thigh and body, the length of the deep layer of the ITB was instead found to be dependent on the length of the TFL.
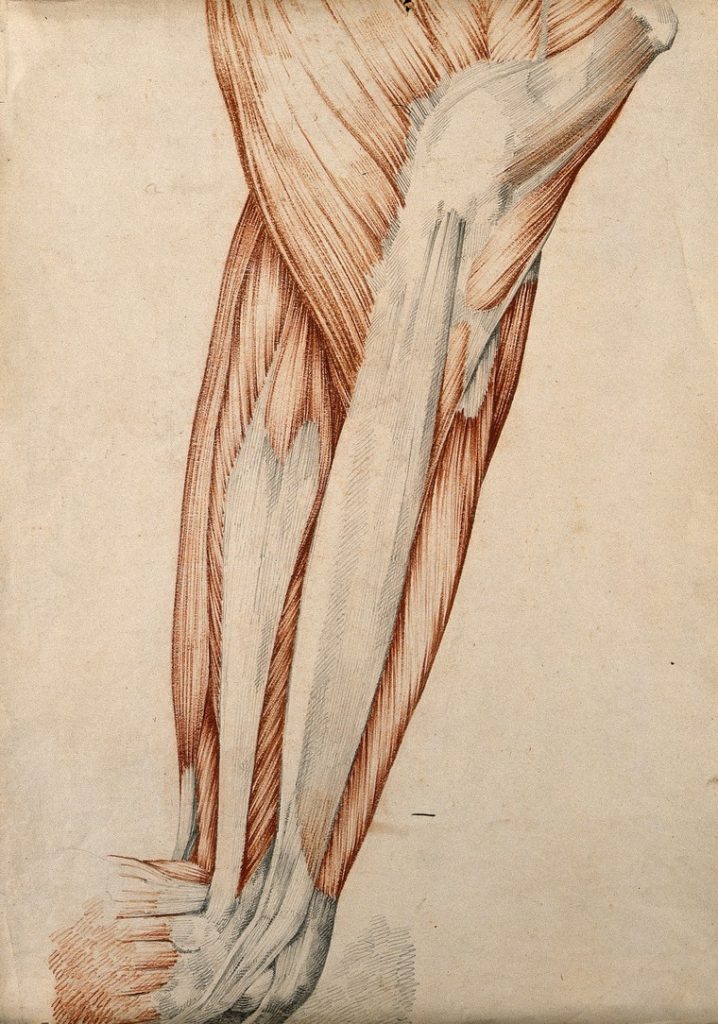
The deep layer of the ITB. From Putzer, D., Haselbacher, M., Hörmann, R. et al. Arch Orthop Trauma Surg (2017). https://doi.org/10.1007/s00402-017-2820-x (Creative Common License)
Conclusion
This research study has given more definitive evidence of not only the existence of the third “deep” layer of the ITB, but also information regarding its morphology, and by extension, its function. This deep layer of the ITB acts both as a second enveloping structure on the deep side of the TFL, as well as a fascial structure that sits over and stabilizes the anterior aspect of the hip joint.
What does it mean?
Read also
- Iliotibial Band Syndrome: ITB cannot be stretched
- ITB: Empirical evidence is the reality—Robert Baker
- ITB: Extrapolating results from research to hands-on manual therapy should be done with caution—Joe Muscolino
- ITB: Our methods still get results; it’s our explanations that need updating —Til Luchau
- Can you stretch the ITB?
This blog post article was created in collaboration with Joe Muscolino


