The Effect of Manual Therapy on COPD
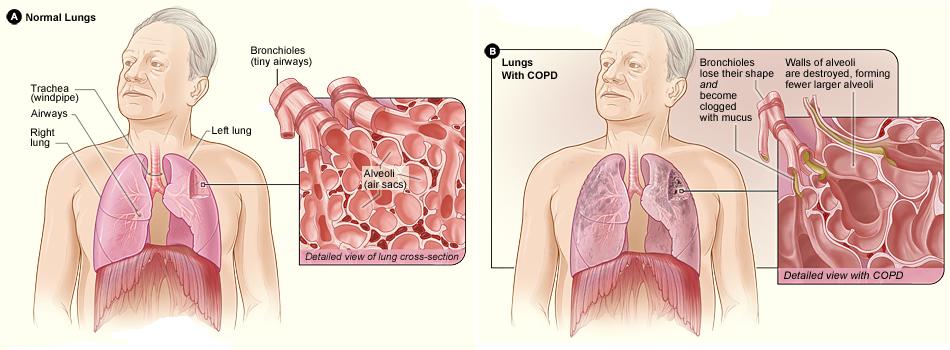
Chronic obstructive pulmonary disease (COPD) is a respiratory condition characterized by progressive airflow limitation that is associated with an inflammatory response
The Effect of COPD on Breathing
COPD causes expiratory flow limitation (difficulty breathing out) and air trapping (residual air left in the lungs), known clinically as dynamic hyperinflation. This phenomenon leads to increases in expiratory reserve volume (amount of air that can be breathed out) and residual volume (air left in the lungs after having breathed out). This in turn results in a negative impact on inspiratory capacity, which can alter the position of the ribs causing a state similar to sustained inspiration over time, often referred to as inspiratory block.
The Effect of COPD on Posture
COPD can manifest as “barrel chest.” In this state, the position of the diaphragm is flattened and shortened reducing its ability to generate force (normally the diaphragm is dome-shaped). As a result, accessory respiratory muscles are recruited as a compensatory adaptation leading to overactivation and shortening of these muscles over time as well. The surrounding cervicothoracic fascia contracts producing postural distortion changes, such as increased thoracic kyphosis, decreased lower to middle cervical lordotic curve, increased extension (lordosis) of the atlanto-occipital joint with concomitant anterior projection of the head, protraction of the shoulder girdles, and internal rotation of the shoulder (glenohumeral) joints. All in all, these changes contribute to an increase in chest tightness and an increase in the amount of effort required to breathe.
Diaphragm

ANTERIOR VIEW OF THE DIAPHRAGM. PERMISSION JOSEPH E. MUSCOLINO. THE MUSCULAR SYSTEM MANUAL – THE SKELETAL MUSCLES OF THE HUMAN BODY, 4TH EDITION (ELSEVIER, 2017).
The diaphragm is the primary muscles of inspiration. In a healthy person, no other muscle is needed to breathe in gently. When a person is healthy, no muscle is needed to breathe out gently because relaxation of the diaphragm and elastic recoil of the soft tissues of the abdomen and thoracic region is all that is needed. However, when we want to breathe in or out forcefully and/or a person is unhealthy, accessory muscles of respiration are recruited.

INFERIOR VIEW OF THE DIAPHRAGM. PERMISSION JOSEPH E. MUSCOLINO. THE MUSCULAR SYSTEM MANUAL – THE SKELETAL MUSCLES OF THE HUMAN BODY, 4TH EDITION (ELSEVIER, 2017).
Accessory Muscles of Respiration
- Accessory muscles of respiration can be divided into accessory muscles of inspiration and accessory muscles of expiration.
- Accessory muscles of inspiration essentially all attach onto the rib cage and have their other attachment situated more superiorly.
- Accessory muscles of expiration essentially all attach onto the rib cage and have their other attachment situated more inferiorly.
- Accessory muscles of inspiration include the scalenes, pectoralis minor, sternocleidomastoid, levatores costarum, and serrates posterior superior.
- Accessory muscles of expiration include the quadratus lumborum, subcostales, serratus posterior inferior, and muscles of the anterior abdominal wall.
- Intercostal muscles are involved in both inspiration and expiration.
Treatment of COPD
Current COPD management strategies include physical activity and respiratory muscle training. Manual therapy is being sought as a way to alleviate these changes. Thus, a study from Chile measured the immediate effect on lung function following a soft tissue treatment in patients with severe COPD. The study was published in International Journal of Chronic Obstructive Pulmonary Disease.
Study
Twelve medically stable patients (n=12) with an existing diagnosis of severe COPD were included. The mean age of the patients was 62.4 years (range 46–77 years). Nine were male and three were female. Residual volume, inspiratory capacity, and oxygen saturation were recorded immediately before and after administration of the soft tissue therapy. The manual therapy protocol was designed to address changes in the accessory respiratory muscles and their associated structures. The treatment was approximately 30 minutes, consisting of treatment of the soft tissues of the chest wall.
Results:
Manual therapy resulted in:
- residual volume decrease from 4.5 to 3.9 liters
- inspiratory capacity increase from 2.0 to 2.1 liters
- oxygen saturation increase from 93% to 96%
Conclusion:
The authors concluded that a single application of soft tissue manipulation appears to have the potential to produce immediate clinically meaningful improvements in lung function in patients with severe and very severe COPD.
This article was created in collaboration with Dr Joe Muscolino