The mechanism of muscle blood flow increases due to massage
There is a myth that massage cannot increase blood circulation, and blood flow is only controlled by heart output. A real understanding of science would tell you otherwise. A review clarified the mechanism.
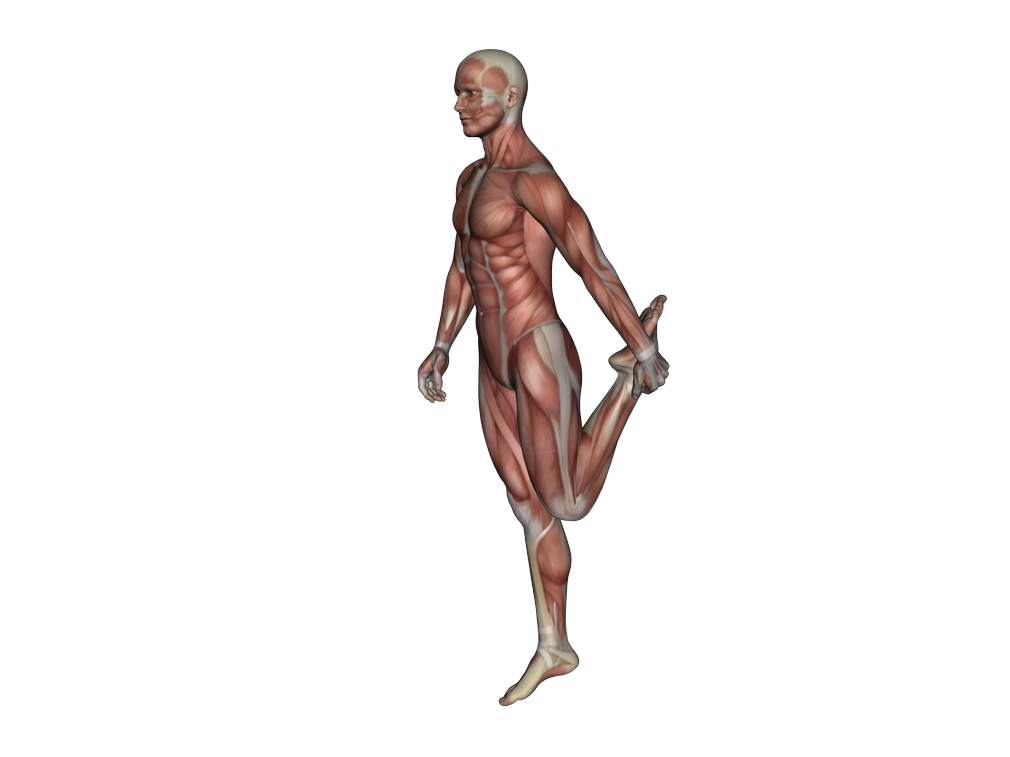
Skeletal muscles while at rest, have a low muscle blood flow, constitutes approximately 20% of cardiac output. While during intensive exercise, about 80% of the total blood flow is directed to skeletal muscles to supply oxygen and nutrients. Metabolic and neural regulation coordinate the large muscle blood flow. While the low muscle blood flow during rest is partly due to the tonic activity of sympathetic vasoconstrictors innervating the muscle blood vessels.
The term muscle vasodilation refers to the widening of blood vessels, which results from relaxation of smooth muscle cells within the vessel walls. While vasoconstriction is the opposite, the narrowing of blood vessels.
It is also known and proven, that somatosensory stimulation (such as massage, stretching, acupuncture or others) can increase muscle blood flow. Many evidences show that massage can increase local blood flow.
Now, researchers from Japan provide some theories on the mechanism in a review paper published in Autonomic Neuroscience .
Increase muscle blood flow via somatosensory stimulation, such as pressure, heat, or painful stimulus to the skin, have been documented in animals and human studies. Somatosensory stimulation excites the afferent fibres in the skin as well as the underlying muscles, joints, connective tissue, and blood vessels. These stimulate mechanoreception, chemoreception, thermoreception, and nociception, and the information is transmitted to the central nervous system (CNS) by afferent fibres. The population of unmyelinated afferent fibres which carry somatosensory information comprises nearly 50% of all cutaneous and muscle afferent fibres.
Somatic stimulation can increase local muscle blood flow can be called by antidromic and local vasodilation. The authors provided several mechanisms of increased muscle flow due to somatic stimulation:
- Many smooth muscles can contract and dilate without neuronal activation, contraction due to muscular origin is known as myogenic tone.
- The artery, which provides blood to skeletal muscles, consists of three different layers, i.e., the outermost layer (connective tissue), middle layer (smooth muscle cells and elastic fibres), and innermost layer (endothelial cells). Among these cells, the endothelial cells have a significant influence on smooth muscle dilation.
- Substances such as ACh, ATP, SP, and CGRP, act on endothelial cells which release nitric oxide (NO). NO is a strong vasodilator. Vascular endothelial cells can release NO following mechanical stimulation.
- Local metabolic substances are also important. Decrease of O2 or increase of CO2 in the tissue or blood can dilate the vascular smooth muscle.
- Circulating hormones, such as adrenaline and atrial natriuretic hormone, dilate the vascular smooth muscle. The increased circulating adrenaline by somatic stimulation may influence muscle blood flow in the body.
General exercise mainly increases muscle blood flow of the entire body so-called reflex pressor response, while antidromic and local vasodilation is limited to the peripheral of the stimulated atea.
It is impossible to regulate muscle blood flow by our minds, but somatic stimulation can create local vasodilation, which can be used to treat patients who have muscle stiffness, muscle pain and are suffering from cardiovascular or other conditions which restrict movement.
Antidromic vasodilation occurs in the resting state and occurs independently of arterial pressure. Thus, physical stimulation to the local part of the body applied in patients who have been confined to their beds for a long time or suffer from cardiovascular disease can help decrease muscle atrophy.
Til Luchau’s comments: