The sacroiliac joint: Victim or culprit
Sacroiliac pain, stability, and dysfunction are separate clinical concepts that should not be mixed.
Sacroiliac joint (SIJ) is known as a pain generator, and is attributed as a cuause in 10-30% of low back pain cases. SIJ dysfunction also caused groin and thigh pain. An estimate that 44% of cases of SIJ pain are associated with trauma onset but the aetiology is still unclear. There are many theories on the cause of SIJ pain; however there is still a lack of general consensus. James Booth and Samuel Morris from the UK write a review in Best Practice & Research Clinical Rheumatology, February 2019 issue, to clarify whether the sacroiliac joint is the primary source of pain or dysfunction.
Anatomy and function of the sacroiliac joints
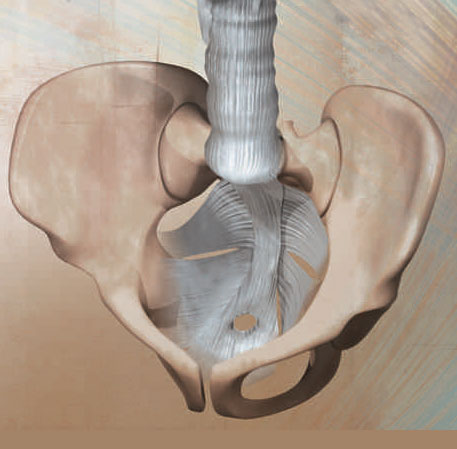
SIJ plays a vital role in transferring loads between the spine and lower limbs acting as stress relievers in the force-motion relationship between the spine and legs. Small amounts of motion can occur in the SIJ acting as a shock absorber between the lower limbs and spine.
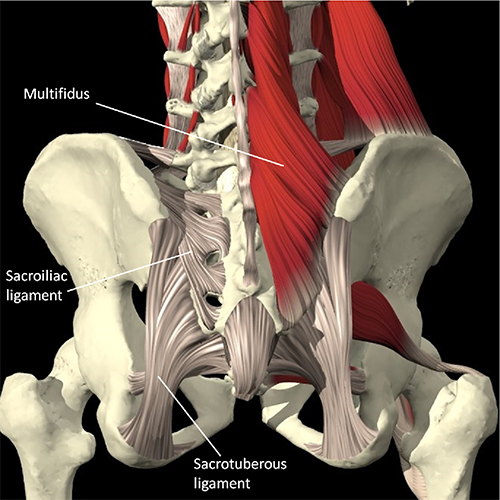
Andre Vleeming and colleagues introduce the concept that to effectively transfer load through the pelvic girdle, it depends on the optimal function of the bones, joints and ligaments (form closure) , optimal function of the muscles and fascia (force closure), and appropriate neural function (motor control, emotional state).
Form closure refers to how the bony and cartilaginous morphology of the SIJs interlocked and contribute to joint stability. Force closure refers to how muscles, ligaments, and fascia contribute to SIJ stability by generating compressive joint forces that are adaptable to changes in loading conditions.
Impairment
Contemporary views of SIJ dysfunctions that may lead to SIJ pain include impairments in SIJ force closure and maladaptation resulting from lumbar and lumbosacral joint fusion.
The primary causes of impairment to the force closure mechanism of the SIJs are considered to be trauma, laxity of the pelvic ligaments, biomechanical asymmetry and suboptimal motor control of associated muscles. Altered joint stiffness and impaired motor control of deep muscles have been associated with lumbopelvic pain. However, studies on impaired motor control are mostly on peripartum women with SIJ pain. In this case, reduced joint stiffness at the SIJ could be due to the effect of sex hormones on collagen synthesis and ligamentous tension.
There are also cases where SIJ is being discussed both as a source of neuromotor abnormalities causing pain in neighbouring structures and as a source of pain caused by neuromotor abnormalities in the same neighbouring structures, the ‘victim and culprit’. The authors added that the force transmitted across the SIJ could be amplified by internal and external factors.
Summary
Based on the review, the authors provide the following summary:
- Sacroiliac pain, stability, and dysfunction are separate clinical concepts that should not be mixed.
- The association of altered sacroiliac stability and pain has been mostly demonstrated in peripartum women where joint stiffness is asymmetrical. This finding has not been adequately reproduced in other population with SIJ pain, including athletes.
- Potential causes of SIJ pain in athletes may be both extrinsic (e.g., training practices causing loading asymmetries in the axial skeleton) and intrinsic (e.g., post-traumatic ligament incompetence or persistent altered lumbopelvic muscle tone following injury to local and neighbouring tissues).
- Due to the highly integrated nature of SIJ function, intrinsic influences on the force closure mechanism may include the lumbar spine, the hip, the knee, the rib cage, and even the shoulder. In this complex and dynamic system, the question of ‘victim’ and ‘culprit’ is perhaps less important. Extrinsic influences include sport-specific movements and adverse or asymmetric loading patterns in the pelvis.
- Biopsychosocial assessment is recommended to further consider the possible influence of cognitive and behavioural influences in producing maladaptive movement patterns, excess muscle contraction and dysfunctional attitudes towards pain and recovery. SIJ pain in the athlete may be associated with trauma or repeated training activities.
- Clinical evaluation should include clustered pain provocation testing. Palpation and mobility testing are still too subjective. Clinicians should avoid using the term ‘instability’ of the joint, which may cause unintended negative effects, particularly in the athletic population.
- Manual therapy has been shown to alter muscle tone and EMG activity in the muscles related to SIJ stabilisation: hamstrings, quadriceps, and abdominal muscles. Moreover, there is also supporting evidence to show an effect on segmental excitability of the central nervous system. However, manual therapy does not necessary affect the structure; the resulting analgesic effects are more likely to be produced by inhibitory neurophysiological responses in the central and peripheral nervous system and via alterations in reflex motor activity.