The spine: Its role in movement and musculoskeletal pain
Freedom to Move by Jo Key integrates applicable contemporary science around spinal movement and pain with clinical evidence and understanding gleaned from the author’s longstanding practice.
This article is an extract from Freedom to Move, Movement Therapy for Spinal Pain and Injuries by Josephine Key (copyright Handspring publishing)
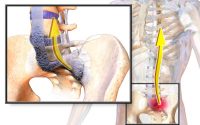
The spine is one of the most complex structural and functional regions of our body and is involved in every activity and movement we do. When it functions well, we feel good, look good, and can perform well. On the other hand, it is also a major source of musculoskeletal pain, the increasing incidence of which represents a burgeoning and expensive problem.
The medical model has not been very successful in treating spinal pain because it looks for structural pathologies in order to diagnose the cause. Yet we know that structural problems – “slipped disks,” tears and the like – do not always occur, or, if they are found, maybe incidental to the pain. Not being able to find a particular cause for a problem limits finding a solution. Most back pain is usually diagnosed as “non-specific”; hence treatment has largely also been non-specific, and had limited results.
A malfunctioning spine is not only the cause of most back pain, it can also be a major source of, or contributor to, many other musculoskeletal pains and injuries – both directly and indirectly.
If we are to better understand and more effectively treat spinal pain, we need to consider how well the spine functions – to appreciate the different qualities of its control in both health and disease. Simply looking at how the spine is supported, and moves can indicate altered segmental loading patterns and likely repetitive tissue stress over time, and thus provide valuable insights into why the pain may have arisen.
The spine is commonly the victim in many exercise and fitness regimens.
The quality of spinal control as we go about our daily lives determines both the state of the spine’s health and the level of our general well-being. If our habitual movements are physiologically sound, we can perform well and participate in most exercise without pain or injury – but have you noticed how many people cannot?
A standard question I ask in taking my initial history with the client is: “what exercise do you do?” More often than not, I discover that elements of their training program, involving some – if not all – of their exercises (including stretches) are directly contributing to the development and/or perpetuation of the problem for which they are seeking help. Unfortunately, this can be particularly so in the case of elite athletes.
In Freedom to Move, I hope to increase the understanding of what constitutes healthy torso movement – to support the functional demands on the spine – and how this is changed in people with pain. With a clearer picture of what is wrong, we are in a better position to prescribe exercise and movement that will restore function without pain.
How effective are exercise interventions for spinal pain?
It is generally accepted that if you have musculoskeletal pain, you should exercise. Maher (2004) pointed out that while exercise was considered to be one of the few evidence-based treatments for chronic back pain, there was uncertainty about which exercises were the most effective and how they should be prescribed. This is still the case, although there has been more relevant research in recent years.
The randomized controlled trial (RCT) is considered the gold standard for judging the benefits of treatments, without bias – and especially when the results from groups of trials are subjected to systematic review and meta-analysis (such as by Cochrane contributors) to answer a particular research question.
However, the exclusive use of quantitative approaches, such as RCTs, can risk a narrow understanding of the subject, and there are progressively more calls to increase the number of qualitative research studies, which generate a different sort of knowledge (Petty et al. 2012). The reductionism in research does not necessarily allow us to fully understand complex biological systems, particularly the movement system. And bear in mind that most subjects in an exercise control group are classed as “normal” because they do not (yet) have pain, which does not necessarily mean that they function well or move optimally.
Physiotherapy-related research
Early research into back pain treated exercise as a generic intervention and the content of the exercises given was usually not described, and neither was the rationale for their inclusion. Unsurprisingly, the results were disappointing. For studies to be useful and have clinical relevance, sufficient detail of the exercises is needed.
As spinal pain research is increasingly finding a substantial association between pain and altered control of posture and movement, there are an increasing number of studies testing the effectiveness of what are known as motor control exercises (MCEs). The results are equivocal.
In chronic low back pain (LBP), MCEs were found to be superior to minimal intervention, but compared with graded activity, there were no significant differences (Macedo et al. 2012). Two Cochrane systematic reviews (Saragiotto et al. 2016; Macedo et al. 2016) again found that MCEs were only “probably more effective than minimal intervention.” More importantly, for both acute and chronic LBP patients, no clinically important difference was found between MCEs and other forms of exercise.
In the case of neck pain, Michaleff et al. (2014) measured “comprehensive physiotherapy exercise” (specific MCEs and sensorimotor training, progressing to functional whole-body exercise) against simple advice for chronic whiplash disorders. Advice was found to be equally as effective as the exercise program.
A proposed solution to the poor treatment outcomes has been to attempt to identify patient subgroups and match them with more targeted exercise therapies. These studies have assigned patients to subgroups on the basis of observation, movement testing, and pain provocation. The most popular subgroups are the McKenzie method, Sahrmann’s Movement System Impairment model and the O’Sullivan classification system. Both the Sahrmann and O’Sullivan models adopt an MCE approach to restoring functional movement.
To date, the O’Sullivan model is showing more favorable outcomes. Vibe Fersum et al. (2013) tested cognitive functional therapy (O’Sullivan’s approach integrates both cognitive strategies and functional rehabilitation to change provocative movement and cognitive behaviors that provoke and maintain pain) against traditional manual therapy and exercise (either “general” exercise or MCE involving isolated contractions of the deep abdominal muscles). The cognitive functional therapy cohort demonstrated superior outcomes. However, one has to question what proportion of the outcome was due to the functional movement/exercise as opposed to cognitive-behavioral therapy?
A further RCT on a particular O’Sullivan LBP subgroup compared a tailored MCE program with general exercise and found “no additional benefit of specific exercises targeting motor control impairment” (Saner et al. 2015). A further study on the O’Sullivan system (Lehtola et al. 2016) tested specific MCE and control of movement patterns against general exercise combined with manual therapy and only found that “MCE may be superior to general exercise.”
In summary, patient subgrouping, where exercise therapy is more tailored to the needs of a specific patient group, could be leading to more positive outcomes. A recent systematic review, however, reveals that the credibility of subgroup claims in LBP trials was low (Saragiotto et al 2016a), which gives us food for thought.
More work is needed. In respect to posture-movement dysfunction, it is clinically apparent that there is less heterogeneity than is generally understood. I have previously proposed (Key et al 2008; Key 2010) that two principal patient subgroup clusters are clinically apparent (albeit with common posture-movement problems also), and that tailoring remedial exercise to these groups is clinically effective. These are described in Chapter 3 of Freedom to Move.
Pilates
This popular fitness exercise program has been heavily adopted in clinical practice for treating LBP, and hence is attracting a lot more research.
Again, the results are equivocal. A systematic review (Lim et al 2011) comparing Pilates to other forms of exercise concluded that Pilates was better than no intervention but not superior to other exercise. The authors noted the relatively low quality of existing studies at that time. Although one RCT comparing Pilates to general exercise (Mostagi et al 2015) found no between-group differences for pain and functionality, when analyzed over time, the general exercise group showed increased functionality and flexibility. A Cochrane systematic review by Yamato et al (2015) found low-to-moderate quality evidence that Pilates is more effective than minimal intervention, but there was no conclusive evidence that it is superior to other forms of exercise.
Yoga
With its ancient traditions and focus upon physical postures, breathing techniques, relaxation, and meditation, yoga can be considered the forerunner of a biopsychosocial approach. Despite many people self-selecting yoga as a means of dealing with their back pain, it is not without its faults.
Eligible RCTs testing the effectiveness of yoga are far from numerous, thereby limiting the power of meta-analysis. Two allied RCTs, however, compared the results of practicing yoga against using a self-care book and conventional exercises and stretching (Sherman et al. 2011) for chronic LBP. There was no difference between the exercise groups, although yoga was shown to be superior to a self-care book.
A systematic review and meta-analysis of yoga for back pain (Cramer et al. 2013) found strong evidence for short-term effectiveness and moderate evidence for long-term effectiveness of yoga for LBP, but none to suggest that yoga is more effective than other exercise programs. Another meta-analysis (Holtzman and Beggs 2013) found that post-treatment, yoga had a medium-to-large effect on functional disability and pain. However, these authors cautioned against overinterpretation of these results, owing to the small number of RCTs, methodological concerns, and the need for further RCTs to compare yoga with an active control group. A Cochrane review of yoga treatment for chronic non-specific LBP (Wieland et al. 2017) suggested little or no difference between yoga and non-exercise with regard to back-related function.
Summary
There are no clear winners – no single form of exercise is superior to another. RCTs on each stream of exercise generally report some improvements against “usual care”. Still, they are not shown to be superior when compared to another form of exercise – indicating that keeping active by whatever means is better than doing nothing. The O’Sullivan model of patient subgrouping and cognitive functional therapy suggests more promising treatment outcomes for back pain, although this approach to exercise therapy alone was not necessarily superior.
In Freedom to Move, I attempt to shed further light upon patient subgroups and offer a more tailored approach to exercise therapy. The common movement faults are described in Chapter 3 of Freedom to Move, and the remaining chapters offer a method of exercise which addresses these faults and restores meaningful function.
This article is an extract from Freedom to Move, Movement Therapy for Spinal Pain and Injuries by Josephine Key (copyright Handspring publishing)
How can research results help us to improve spinal exercise prescription?
There has been a considerable shift in the focus of back pain research toward a more holistic functional approach since I wrote my previous book in 2008. Here, I will broadly summarize the research which directly pertains to therapeutic exercise.
The important take-home message: The deconditioning paradigm for LBP (loss of muscle strength and endurance and reduced aerobic capacity) is obsolete. Despite the common belief that “if you have back pain, you need to get strong,” there is no conclusive evidence that weakness is related to back pain, or that strengthening alleviates it.
There is, however, a proven lack of neuromuscular ability, with altered adaptive control of movement (Hodges and Smeets 2015) and reduced postural endurance. Following on from his article in 2003 that “relearning” more refined and skilled control and coordination appeared to be more important than strength and endurance training, Hodges (2013) also reported that the significance lay in how the nervous system controls posture and movement.
Research is increasingly looking at how motor control is altered in people with back pain and finding a redistribution of activity within and between muscles (Hodges 2011).
Essentially, there is evidence of atrophy and under-activity and/ or delayed activity in certain “deep” muscles. To compensate for this, some of the “superficial” or “global” muscles are overactive.
This imbalanced activity between the deep and superficial muscles impairs the person’s ability to optimally control the basic functions which underlie all healthy movement – posture and breathing. Movement patterns and their quality suffer.
In general, movement quality deteriorates, becoming coarse and gross, and showing less variety. There is higher superficial muscle co-contraction, higher compressive loading on the spine, and impoverished sensory feedback, and this adaptive motor behavior becomes entrenched through reinforcement learning. The spine becomes stiff – it does not move enough! It loses its “juice,” flexibility, and the ability to fine-tune segmental movements, so postural stability suffers.
These findings challenge the hitherto popular spinal pain treatment paradigm that the spine is unstable and “needs to be stiffened” or strengthened. Importantly, undertaking a strengthening program can reinforce these compensatory movement patterns, negatively impacting the spine and other systems such as the “core.”
This article is an extract from Freedom to Move, Movement Therapy for Spinal Pain and Injuries by Josephine Key (copyright Handspring publishing)