The Transverse Diaphragms
The transverse diaphragms are layers of connective tissues and fascia that run transversely through the body, these layers are perpendicular to the common myofascial planes which run longitudinally through the body. (Diaphragms comes from ancient Greek word diaphragma which means partition).
Anatomically, the transverse diaphragms occurred in certain junction areas of the body. The concept of transverse diaphragms originated in Osteopathy, and have been used in myofascial release and Craniosacral Therapy [1].
Transverse Diaphragms occurred in what is known as transitional zones, or anatomically known as junctions, where the function of the spinal column changes. Osteopath Gordon Zink, DO considered these as the anatomical weak points [2]. Manual therapists have frequently find that these transitional regions are where most fascial restriction, muscular imbalance or somatic dysfunction can be found.
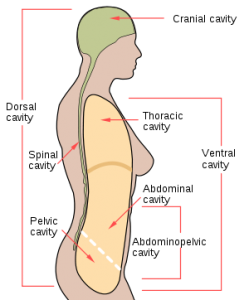
The transverse diaphragms help to compartmentalize different body cavities (Fig. 1). There are 4 major diaphragms in the body: the cranial base, thoracic inlet, respiratory diaphragm, and pelvic floor. They occurred at the junctions where the regions of the vertebrae change function. Each diaphragm is unique, stretches from the front of the body, to the back.
The diaphragm also serves as a ‘dam’ of a membrane or flexible layer that separates one space from another. Manual therapists often find repeated restrictions these areas, and this led to the hypothesis that these diaphragms act as dams which prevent the flow of fluid throughout the body. The transverse layers of connective tissues can inhibit the smoothness of fascial glide that run longitudinally throughout the body.
These areas can augment (when they are functional) or inhibit (when they are dysfunctional) the flow of interstitial fluids. The area of dysfunction constitutes a region where the interstitial fluid is not moving.
Fig 1. Major body cavities found in human. Image from Wikipedia.
Transitional Zones Vertebral Junctions Transverse Diaphragms
Occipital-Atlantal (OA) Craniocervical Tentorium Cerebella
Cervico-Thoracic (CT) Cervicothoracic Thoracic Inlet/Outlet
Thoraco-Lumbar (TL) Thoracolumbar Respiratory Diaphragm
Lumbo-Sacral Lumbosacral Pelvic Diaphragm
The Craniocervical Junction
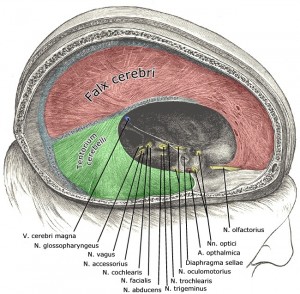
It is a complex articulation between the occiput, atlas, and axis. There is extensive mobility at this junction, the heavy head balances on the supple cervical spine. This is the site of the tonic neck reflexes, which influences postural muscular tone throughout the trunk. If function is disturbed here, it frequently creates hypertonus of the postural muscles, disturbances of equilibrium and locomotor deficits [2]. The tentorium cerebelli (Fig. 2) is found here, it is an extension of the dura mater that separates the cerebellum from the inferior portion of the occipital lobes.
Fig. 2. Tentorium cerebilli (from Gray’s Anatomy & Wikipedia)
The Cervicothoracic Junction
The cervicothoracic junction is the region where the most mobile part of the spinal column is joined to the relatively rigid thoracic spine. It is also where the powerful muscles of the upper extremities and shoulder girdle insert [2].
The thoracic inlet diaphragm covers the superior thoracic aperture( the superior opening of the thoracic cavity). Anatomically it is referred as the thoracic inlet and clinically as the thoracic outlet. This is also where the brachial plexus passes. Impingement of the plexus in the region of the scalenes, ribs, and clavicles is responsible for thoracic outlet syndrome.
Thoracolumbar Junction
At the thoracolumbar junction spinal function changes abruptly as is seen in the differences in the upper (thoracic) and lower (lumbar) joints. Somatic dysfunction in this area can be associated with hypertonus of the iliopsoas, quadratus lumborum, thoracolumbar erector spinae and inhibition of the rectus abdominus muscles [2].
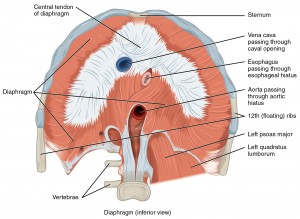
The respiratory diaphragm (or called thoracic diaphragm in anatomy), is found in this transitional zone (Fig. 3). The diaphragm separates the thoracic cavity (heart, lungs & ribs) from the abdominal cavity and performs an important function in respiration. Contraction and relaxation of this diaphragm provide the function for breathing and it also produces alternating intrathoracic and intra-abdominal pressure gradients which provide the pumping mechanism for the venous and lymphatic circulation.
Fig. 3. The respiratory diaphragm
“1113 The Diaphragm” by OpenStax College – Anatomy & Physiology, Connexions Web site. http://cnx.org/content/col11496/1.6/, Jun 19, 2013.. Licensed under CC BY 3.0 via Commons.
Lumbosacral Junction
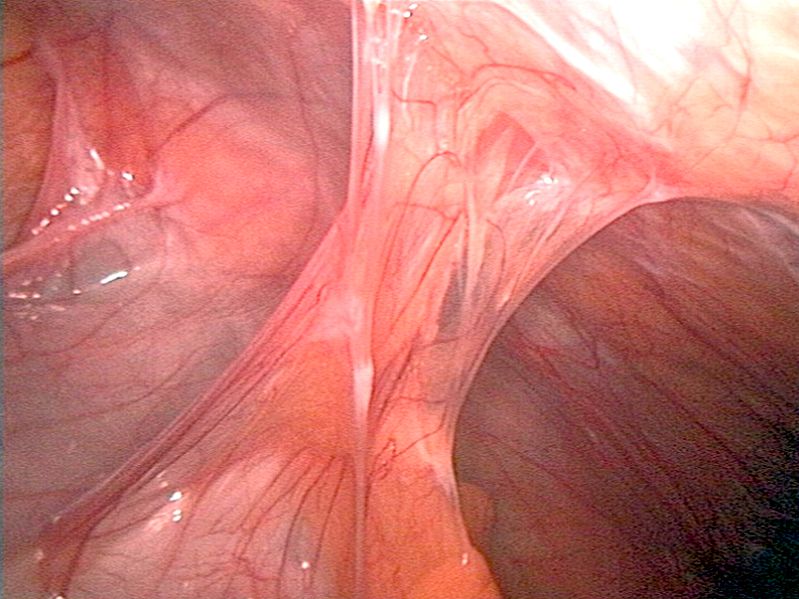
The lumbosacral junction forms the base of the spinal column and is therefore a major determinant of body statics. Movement from the legs is transmitted through this junction to the spine. The pelvic diaphragm or pelvic floor is associated with this junction (Fig. 4). It is composed of muscle fibres of the levator ani, the coccygeus, and associated connective tissue which span the area underneath the pelvis.
Fig. 4. The pelvic floor (from Gray’s Anatomy)
The Eight Diaphragms
The Dallas Osteopathic Study Group have further identified eight diaphragms [3]:
- Plantar fascia
- Knee diaphragm
- Popliteal fascia
- Cruciate ligaments and transverse ligament of the knee
- Pelvic diaphragm
- Respiratory diaphragm
- Thoracic outlet
- Anterior cervical fascia
- Subclavius muscles, costocoracoid ligaments and costoclavicular ligaments
- Suboccipital triangle
- Tentorium cerebelli
- Diaphragm sellae
In myofascial release, the function of the diaphragms is evaluated by feeling for the quality—its volume and smoothness of flow—of the tide flowing through each diaphragm. The amplitude and the quality of the tide is more important rather than its frequency. Myofascial release aims at removing the “obstructions” to the flow of the interstitial fluid, which allows the tide to move more smoothly and at its optimum amplitude [3].
The myofascial release technique for each diaphragm is basically the same, only with a modification of the position of the therapist’s hands. Place one hand below the area (under the client) and one hand over the area of the diaphragm. Apply a gentle pressure focussing on the diaphragm, and follow any inherent tissue motion. It is important not to allow the tissue to go back in the direction from which it has just moved. This hold will produce a softening and lengthening of tissues. Sometimes it can increase the breath, build-up of heat, and stomach gurgling. It can also encourage unwinding or unconscious movement of limbs. When a pulse, or energetic repelling is felt, it signals that the release is complete and the therapist should remove their hands. Often the signs of completion are a dramatic sigh, but just as often, a simple feeling on the part of the therapist that they are “complete” at that spot and their hands should move on to another location [3]. This myofascial release treatment aims to decreases tissue hypertonus, promotes energy and fluid exchange, and restores mobility and balance to their constituent structures.
References
[1] Kailas, Transverse Diaphragm Release in CranioSacral Therapy. Available from http://craniosacraltopics.blogspot.com/2008/12/transverse-diaphragm-release-in.html
[2] Pope, R.E. (2005) The Common Compensatory Pattern: Its Origin and Relationship to the Postural Model. In: Erik Daltion, Advanced Myoskeletal Alignment Techniques, Freedom from Pain Institute.
[3] Speece, C.A., Crow, W.T. (2001). Ligamentous Articular Strain: Osteopathic Manipulative Techniques for the Body. Eastland Press.