Understanding the Placebo Effect
Understanding The Placebo Effect by Brian Fulton RMT
Some therapists shudder at the mention of the term placebo effect, others are curious as to what it might be, still others embrace the concept. Where do you lie on this spectrum? Sticking one’s head in the sand and denying that it exists in your treatments is actually not helpful to you or to the patient, because the placebo effect has been found to exist in virtually every medical encounter and appears in virtually almost every drug trial ever performed.
“There is no ‘choice’ about whether or not to ‘use’ the placebo (and nocebo) effects. Those effects are going on in every medical encounter between patient and physician. They exist whether we want them to or not; whether we are consciously exploiting them or not. The ‘choice’ is about how we go about using them: well or poorly, blindly or thoughtfully.[i] – Dr. Howard Brody, Director of the Institute for Medical Humanities of the University of Texas.
In 2011, the Journal of Manual and Manipulative Therapy published a peer-reviewed paper published by entitled ‘Placebo response to manual therapy: something out of nothing?’ In it, the authors look at 94 different research papers on manual therapy and on the placebo effect and draw some relevant inferences about the placebo effect in manual therapy. Some of the papers that they looked at clearly suggested that what you and I think may be happening isn’t exactly what is happening. The evidence points to a strong placebo component in what we do in the manual therapy professions. The authors state the following:
“We suggest that manual therapists conceptualize placebo not only as a comparative intervention, but also as a potential active mechanism to partially account for treatment effects associated with manual therapy. We are not suggesting manual therapists include known sham or ineffective interventions in their clinical practice, but take steps to maximize placebo responses to reduce pain.” [ii]
Another review of evidence is a paper published in 2010 entitled Effectiveness of manual therapies: the UK evidence report. In this report the authors looked at 49 recent relevant systematic reviews, 16 evidence-based clinical guidelines, plus an additional 46 random controlled trials (RCT) that had not yet been included in systematic reviews and guidelines. The authors looked at 26 categories of conditions containing RCT evidence for the use of manual therapy: 13 musculoskeletal conditions, four types of chronic headache and nine non-musculoskeletal conditions. This report, published in Chiropractic and Manual Therapies (the official journal of the Chiropractic & Osteopathic College of Australasia, the European Academy of Chiropractic and The Royal College of Chiropractors) recognizes the important role that manual therapy plays in treating a wide variety of ailments, but even in this report the authors state:
“Additionally, there is substantial evidence to show that the ritual of the patient practitioner interaction has a therapeutic effect in itself separate from any specific effects of the treatment applied. This phenomenon is termed contextual effects. The contextual or, as it is often called, non-specific effect of the therapeutic encounter can be quite different depending on the type of provider, the explanation or diagnosis given, the provider’s enthusiasm, and the patient’s expectations”[iii].
Research interest in this phenomenon has continued to grow dramatically in this topic. In 2011 Harvard created an institute dedicated wholly to the study of placebos, the Program in Placebo Studies and the Therapeutic Encounter (PiPS). It is based at the Beth Israel Deaconess Medical Center and Ted Kaptchuk, a prominent figure in placebo studies, was named its director. Its purpose is to bring together researchers who are examining the placebo response and the impact of medical ritual, the patient-physician relationship and the power of imagination, hope, trust, persuasion, compassion and empathic witnessing in the healing process. PiPS research is multi-disciplinary extremely inclusive spanning molecular biology, neuroscience and clinical care, as well as interdisciplinary, ranging from the basic sciences to psychology to the history of medicine. This certainly gives you an idea of not just how important the study of the placebo effect is, but also how complex it is.
If one looks at the money and energy that is now being invested in understanding the placebo effect, it is clear that the study of this innate healing phenomenon has come of age; and yet the term drags centuries of baggage along with it. In common language people will often say, “Oh, that’s just a placebo effect.” What people often fail to recognize is that every time the placebo effect is observed, the body is healing itself. Is this not our goal as health practitioners? Is it not our primary goal to help create an environment where the patient’s body can heal itself? I submit that the primary reason for practitioners to understand the placebo effect is so that we can learn to manage the contextual factors within the clinical environment that will couple with our physical intervention to produce an optimal healing environment.
What is the Placebo Effect?
Admittedly most of our knowledge surrounding the placebo effect is theory. What is not known vastly overshadows what is known, but the working theory is that psychosocial cues initiate neurobiological mechanisms which modulate existing healing responses, bringing about subjective and objective (measurable) changes.
— The Placebo Effect —
Psychosocial Cues -> Neurobiological Pathways -> Subjective and Objective Changes
Psychosocial Cues
Cues in the environment and in the patient-practitioner relationship appear to trigger placebo effects. A common term that you have undoubtedly encountered for these cues is contextual factors. This is a very useful term as it alludes to what might be going on. Another term used to describe this phenomenon is non-specific effects however, not only does this term lack any real description or hint as to what is going on; it is actually misleading. A far cry from non-specific, the ‘effects’ of this phenomenon can be amazingly specific: from blood pressure changes, changes in immune response, improvement in exercise tolerance, or changes in tissue quality to name just a few. What are more elusive and complex are the triggers and the pathways that bring about this effect. While semantics get raised every time the placebo is discussed, I suggest that we not get side-tracked by semantics, but rather focus on the factors that initiate this healing phenomenon.
The triggers for these healing effects are wide and varied (as are humans) but there is some agreement that they can be grouped under one of the following the headings: conditioning, expectancy, and meaning. Meaning is a very broad topic though that takes in a large number of concepts. The following is a list of concepts that I examine in my book, The Placebo Effect- Improving Clinical Outcomes. Research supporting each concept is examined in the book, and practical methods are discussed for incorporating each idea into one’s own practice to the end of improving clinical outcomes. [iv]
Examples of Psychosocial Cues (Contextual Factors)
- Expectancy (Hope, Belief)
- Conditioning
- Trust in the Practitioner
- Motivation and Desire
- The Power of Listening
- Feelings of Care and Concern from Practitioner
- Establishment of a Feeling of Control
- Reducing your Patients’ Anxiety Levels
- Receiving Adequate Explanation of the Pathology
- Acceptance of the Mystery of Healing
- Certainty of the Patient
- Time Spent By the Practitioner
- Use of Ritual
- Professionalism
- Clinician’s Belief System
- Confidence of the Practitioner
- Competence of the Practitioner
- Practitioner’s Attire
- Enthusiasm of Practitioner
- Use of Humour
- Patient’s Inner Narrative
- Clinical/Healing Environment
Every factor listed above has been shown to independently affect clinical outcomes, and there is likely an additive healing effect from these cues. Becoming aware of these elements in your daily practice and consciously improving your skills in these areas will yield benefits for the patient. Ultimately these contextual factors are what we need to focus on is we want to manage placebo triggers in the clinical environment. A complete article could easily be devoted to every one of these contextual factors. For more information on each of these topics I recommend reading ‘The Placebo Effect in Manual Therapy-Improving Clinical Outcomes’.
Pathways and Mechanisms
“On the basis of these recent insights, it is clear that the placebo response represents an excellent model to understand mind-body interactions, whereby a complex mental activity can change body physiology. Psychiatry and psychology, as disciplines investigating mental events, are at the very heart of the problem, for they use words and verbal suggestions to influence the course of a disease. Psychiatry, for example, has in its hands at least two therapeutic tools: words and drugs. Interestingly, what has emerged from recent placebo research is that words and drugs may use the very same mechanisms and the very same biochemical pathways.”[v]– Fabrizio Benedetti (Professor of Physiology and Neuroscience at the University of Turin Medical School)
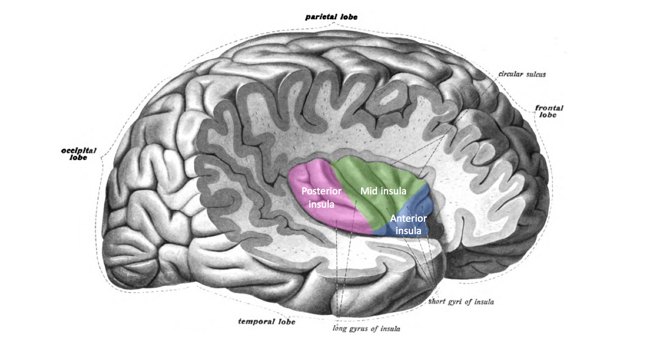
What is known for sure about placebo pathways is that if an individual lacks prefrontal control, there is limited to no placebo response. The prefrontal cortex is brain region is intimately involved in planning complex cognitive behavior, personality expression, decision making, and moderating social behavior. This brain region is considered to be the centre of orchestration of thoughts and actions in accordance with internal goals. One of the features of Alzheimer’s disease is the impairment of prefrontal executive control. Benedetti found a clear disruption of the placebo response occurred when reduced connectivity of the prefrontal lobes with the rest of the brain was present.[vi]
At least four biological pathways have been proposed for facilitating placebo responses.
Endorphin Pathways– Diagnostic equipment now allows us to look inside of the living brain and see what is going on. Brain scans show µ-opioid receptors in the brain being activated by a placebo in brains of subjects experiencing pain relief from taking a placebo.[vii] Clearly the endorphin pathway is involved in the placebo effect, especially where pain modulation is happening.
Neuroendocrine Pathway– The neuroendocrine pathway involves not just the sympathetic and parasympathetic nervous systems, but also the hypothalamus, pituitary gland and the adrenal glands, collectively known as the HPA axis. The neural pathway of the HPA axis signals the adrenal medulla to release catecholamines (not the least of which is adrenaline), which are known to increase heart rate, blood pressure, breathing and metabolic rate. In addition to these symptoms, our sympathetic nervous system increases muscle tone, which as you know can manifest as musculoskeletal pain. Dampening of this pathway (which can be triggered by a thought or a feeling) could account for placebo success with generalized musculoskeletal pain, specific pain such as headaches, cervical or lumbar pain. This pathway is also proposed for placebo success with hypertension, chronic pain and stomach ulcers, as well as immune system bolstering and normalization of blood sugar levels.
Psychoneuroimmune Pathway- Immune system cells are studded with receptor sites for neuropeptides associated with emotional states. In other words, your immune system reacts to (among other things), how you are feeling. There are both afferent and efferent fibres in this pathway, so there is a lot of information passing back and forth from the brain to the immune system allowing for fine-tuning, checks and balances. Involvement of the hypothalamus and pituitary gland in this loop has caused some researchers to speculate that there is an ideal ‘set point’ for the immune system, to keep it at a certain level of readiness[viii][ix]. What we have learned is that conscious intervention can modulate this immune response, much as it does with respiration and blood pressure.
Acute Phase Inflammatory Response- In his book, Placebo: Mind Over Matter in Modern Medicine, Dylan Evans presents a detailed argument for the acute phase inflammatory response theory. Evans states that the conditions where the placebo effect is most pronounced (pain, swelling, ulcers, depression anxiety) all involve the acute phase inflammatory response. He reminds us that this response goes beyond the classic signs of inflammation (tumor, rubor, calor and dolor), but is now recognized to include a suite of symptoms known as ‘sickness behaviour’.[x] Sickness behaviour includes lethargy, apathy, loss of appetite and increased sensitivity to pain.
Subjective and Objective Changes
Not only do people experience substantial pain relief from placebo interventions, studies have seen measurable changes in heart rate, blood pressure, immune response, endocrine response, and inflammation, which can bring about healing responses seen in tissue changes, range of motion, pain levels, exercise tolerance, and even markers such as BMI.
Some examples include:
- A wisdom tooth extraction trial[xi] using placebo ultrasound produced reductions in swelling and healing time.
- Studies have found increase in natural killer cell function with saline injections when subjects where first conditioned with adrenalin injections.[xii]
- Dylan Evans’ list of conditions most influenced by placebos includes: inflammation, stomach ulcers, anxiety, depression and virtually all types of pain.[xiii]
- Investigation into the mechanism of the placebo effect currently taking place at several medical universities has documented substantial, measurable physiological changes taking place.[xiv]
- A 2011 review of current literature conducted by Fabrizio Benedetti stated, “recent research has revealed that these placebo-induced biochemical and cellular changes in a patient’s brain are very similar to those induced by drugs.”[xv]
Ethical Considerations
When one thinks of using placebos, deception often comes to mind, since this is how they have often been used in the past. However in my investigation of contextual effects that elicit the placebo response in the clinical environment, I have found that the exact opposite is true. As I began writing my book I began to see several themes emerge. The first theme is the importance of trust in the practitioner/patient relationship. Anything that enhances this trust will tend to enhance healing responses (and vice versa). Clearly deception will not enhance trust. Secondly, improved healing responses are seen when the locus of control lies with the patient, rather than the practitioner. The patient that takes charge of his or her health is going to see improved outcomes. Making the patient aware that these amazing healing effects exist within their own mind and body do not lead to evaporation of the effect, but to enhancement of healing responses and a personal sense of power over one’s health. Finally, increased professionalism of the practitioner leads to improved placebo responses. This may be a perception issue, since much of the placebo effect appears to involve the patient’s perception of their practitioner, but the way to improve their perception of you is by being a more competent professional. So in the end, if you are an ethical professional, you have no worries about employing techniques to encourage healing in your patients. In fact, I recommend reminding your patients that the placebo effect is real, and it manifests from their own internal healing systems as well as their relationship with you. It is not a minus, but a plus for the patient to realize the amazing healing potential of their own bodies.
Conclusion
I hope that you now see that the placebo effect isn’t quite as mysterious as you may have thought. It manifests from innate healing mechanisms present in the body, and many triggers for this phenomenon appear to flow out of a healthy patient-practitioner relationship. Furthermore, placebo effects are real and often measureable. Our task as practitioners is to understand and optimize contextual factors within the clinical environment that can act as triggers enhancing the patient’s innate healing response. This can be incorporated ethically and seamlessly into each and every treatment during assessment, interaction, and treatment of the patient. Our goal as practitioners should be to become more competent at understanding and managing the complex dynamics known as contextual factors that come into play in the therapist-practitioner relationship.
[i] Using Placebo Responses in Clinical Practice: Is there a there, there? What do we need to know? Samueli Institute, Jan. 20, 2012, pg 15
[ii] Bialosky, J.E et al. (2011) Placebo response to manual therapy: something out of nothing? J Man Manip Ther. February; 19(1): 11–19
[iii] Bronfort, G. et al. (2010) Effectiveness of manual therapies: the UK evidence report. Chiropr Osteopat. 2010; 18: 3.
[iv] Fulton, B. (2015) The Placebo Effect in Manual Therapy- Improving Clinical Outcomes. Handspring Publishing, Edinburgh: 84-246
[v] Benedetti, F (2012) The placebo response: science versus ethics and the vulnerability of the patient. World Psych. 11(2): 70–72.
[vi] Benedetti, F. et al., (2006) The Biochemical and Neuroendocrine Bases of the Hyperalgesic Nocebo Effect. Journ Neurosci, 26(46):12014–12022
[vii] Zubieta et al. (2005) Placebo effects mediated by endogenous opioid activity on µ-opioid receptors. The Journal of Neuroscience 25(34): 7754-7762.
[viii] Schwartz, C. (1994). Introduction: old methodological challenges and new mind-body links in psychoneuroimmunology. Advances in Mind-Body Medicine 10(4): 4-7
[ix] Barak, Y. (2006). The immune system and happiness. Autoimmunity Reviews 5 (8): 523-527
[x] Kent, S., R.-M. Bluthe et al. (1992). Sickness behaviour as a new target for drug development. Trends in Pharmacological Science 13: 24-28
[xi] Hashish, I., H.K Hai et al. (1986). Reduction of postoperative pain and swelling by ultrasound treatment: a placebo effect. Pain 33: 303-311
[xii] Kirschbaum, C et al. (1992). Conditioning of drug-induced immunomodulation in human volunteers: a European collaborative study. British Journal of Clinical Psychology 31: 459-472
[xiii] Evans, Dylan (2004). Placebo: Mind Over Matter in Modern Medicine. London, England. Harper Collin: 44
[xiv] Benedetti F., Amanzio M. (2013). Mechanisms of the placebo response. Pulm Pharmacol Ther. Jan 28. pii: S1094-5539(13)00052-7
also Pollo A, Carlino E, Benedetti F. (2011) Placebo mechanisms across different conditions: from the clinical setting to physical performance. Philos Trans R Soc Lond B Biol Sci. Jun 27;366(1572):1790-8.
also Meissner K. (2011) The placebo effect and the autonomic nervous system: evidence for an intimate relationship. Philos Trans R Soc Lond B Biol Sci. Jun 27;366(1572):1808-17.
[xv] Benedetti, F., Amanzio, M. (2011). The placebo response: how words and rituals change the patient’s brain. Patient Educ Couns. 2011 84(3):413-9.