Unpacking the Frictionless Skin-Fascia Interface
A 2002 Study stated that the skin-fascia interface is frictionless. This was interpreted that in myofascial techniques, we cannot apply a shear force or tension the tissues under the skin because the skin-fascia interface is slippery. We look into what recent studies tell us and demonstrate that taking any theory too far is precarious.
There is “theory” popularized via the social media that because the skin-fascia interface onto underlying bone is frictionless, you cannot mobilize underlying bones unless the force placed into the patient’s/client’s body is perpendicular to the surface of the bone. The reasoning is as follows: because the interface between the skin-fascia and the underlying bone is frictionless, if a force is placed in any direction that is not perfectly perpendicular to the bone (in other words, the force is a shear force that is effectively parallel to the bone), the skin-fascia tissue layer would simply slide along the underlying bone instead of being transmitted into the bone to move/mobilize it. In effect, the theory holds that friction is needed between the fascia and bone in order for the force to be transmitted into the bone to move it.
In addition, the study was interpreted as one can’t affect the fascia and tension a muscle because the skin-fascia interface is frictionless. It is also interpreted that we can’t apply a shear force to tissues under the skin with massage strokes.
A 2002 Canadian study by Bereznick et al was cited as the evidence. Let’s walk through what recent studies say about this.
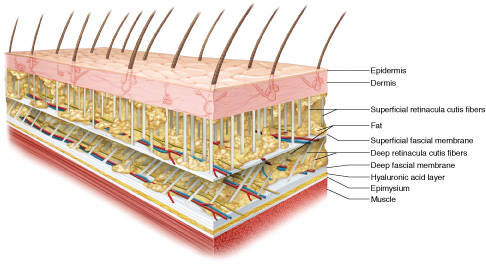
Subcutaneous fascia. Copyright & permission Joseph E. Muscolino. www.learnmuscles.com.
The 2002 Canadian Study
This 2002 Canadian study aimed to evaluate the chiropractic technique of joint mobilization / manipulation which, during thoracic manipulation attempts to apply obliquely oriented force vectors (oblique meaning being between perfectly perpendicular and perfectly parallel to the underlying bone) onto underlying vertebral spinous or transverse processes. As stated above, the premise of the study is that friction is required at the skin-fascia interface onto the bone for the applied shear force to grab/hook the bony process. The study assessed the friction at the thoracic skin-fascia interface onto the bone to determine the force that is actually transmitted onto the bones during thoracic joint mobilization.
Methods
Three male subjects were placed in the prone position with the thoracic skin exposed. The posterior thoracic region was loaded with perpendicular forces, incrementally from 125.3 N to 392.9 N. The interface between the load and the skin was either a plexiglass plate or modelled hands. A force was then applied to either apparatus in the cephalad direction (in other words, a shear force was applied somewhat parallel to the underlying bony contour). The applied forces were measured using a load cell and skin displacements were measured using an infrared camera. As a comparison, the researchers also collected displacement force on a sandpaper, a surface which has friction. In a separate experiment, chiropractors performed actual thoracic manipulation to determine if they could maintain their location of contacts (spinous process/ transverse process) on the underlying vertebra.
Results
The authors found that forces placed into the body over thoracic region was dominated by perpendicular force components, and it was speculated that the shear forces were transmitted to the surrounding skin. They concluded that skin-fascia interface over the thoracic spine exhibits negligible friction, so that during thoracic spinal manipulation, the practitioner cannot direct a force vector to a thoracic vertebra at a given angle by simply directing their thrust in that direction. The application of this study would seem to indicate that only perpendicular forces into bone can effectively move the bone.
The authors also listed various limitations of the study, and provided a caution when applying the findings of this study to other areas of the spine or during other manipulative procedures.
However, some people have taken this small study as definite theory. Greg Lehmann shows in a Youtube video how this theory would be applied to manual therapy. He shows that to open a sliding glass door, one cannot slide their hands along the glass (in effect, a shear force) to move it because if there were no friction, then the force applied would simply slip and slide along the glass instead of transferring that force into the glass to move it (https://www.youtube.com/watch?v=WexdWlfQzaU).
However, the “absolute” manner in which this concept is applied might not be 100% correct for the following three reasons:
- The application of this theory would be true only if the surface interface is 100% frictionless, which a later study (see below) would seem to contradict.
- The movement in the video along the glass is shown as being perfectly parallel to the glass. However, if the force is applied obliquely, in other words anywhere between perfectly perpendicular and perfectly parallel, then the force of that oblique direction could be resolved (resolution of vectors) into the perpendicular force and a parallel force. Whatever % of the force is perpendicular should be able to be transmitted into the bone to move/mobilize it.
- Second, once the slack of the superficial skin-fascia tissue is taken out, then the tension in that superficial tissue would have to be exerted onto underlying deeper structures at their attachment sites. If these attachment sites are anywhere along that bone, then the force would be transmitted into the bone. To be fair, this transmission of force is indirect, which is briefly mentioned in the video as possible, but it is passed over much too quickly.
Application to Soft Tissue Manipulation (Massage)
The authors in the paper also suggested that in soft tissue massage, the practitioner, in some instances, determine the direction of muscle fibres and then apply a stripping type motion to stretch one attachment of the muscle away from its other attachment. This study seems to indicate that this cannot be accomplished due to the frictionless nature of the soft tissue interfaces.
The 2014 American Study
This study was in the context of osteopathic techniques, which usually involve compressive (perpendicular) and tangential (shearing) forces to target the fascia. These forces are transmitted to the skin and adipose tissue before the fascia is encountered. The authors calculated using a mathematical model the extent of deformation of these two tissue layers relative to the fascia.
Based on a mathematical model, the authors found that the compression and shearing forces required to produce a deformation of 9% compression and 4% shear for the skin (the most superficial layer) were 50 N and 11 N, respectively. For adipose tissue (the second layer), these forces were 36 N and 8 N, respectively. Whereas for the underlying fascia (the deepest of the three layers), compression and shearing forces of about 100 N and 22 N were necessary for a similar deformation.
What does this mean?
The authors concluded that the forces applied to the surface of the skin WERE transmitted through the skin and adipose into the fascia. What is most important here is that the “shearing” force did transfer from the skin to the fascia. More force was necessary for the same shear deformation of the fascia compared to the skin to occur (22 N compared to 11 N), but the force did transfer to the fascia.
As the tissues cannot be compressed, they must deform differently in the lateral direction, which implies that the tissue impact in the lateral direction is quite different from that in the perpendicular force to the skin. The authors added that the direction and pressure of the tissue may be important in achieving a desired clinical outcome.
2016 Canadian Study
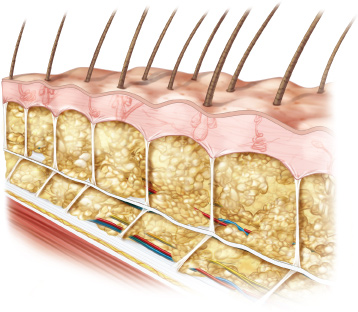
Shearing of subcutaneous fascia. Note the tension in the deeper retinacula cutis fibers. Copyright & Permission Joseph E. Muscolino. www.learnmuscles.com.
A study from Ontario, Canada aims to clarify how loads due to manual therapy are transmitted into deeper tissues of the body. This investigation monitored tissue displacement at sequential depths in thoracic paraspinal tissues parallel with surface load directions (in other words, shear forces).
Now with an advanced ultrasound technology, this study addressed limitations of the 2002 study, which suggested that during a load, only pure perpendicular compression force is transmitted deeper into the body into the bone.
Twenty-four healthy participants were prone and manual therapy shear forces were applied to the body. Ultrasound speckle tracking synchronously monitored displacement and shear deformation of tissue layers in a region of interest adjacent to load application to a depth of 4 cm. Cumulative and shearing displacements were quantitatively estimated. The results show that the cephalocaudal cumulative displacement in layers parallel to the surface were, in order of depth, 1.27, 1.18, and 1.06 mm, respectively. The superficial/intermediate shear was 2.1 ± 2.3% whereas the intermediate/deep shear was 4.4% ± 3.7.
What Does This Mean?
Both Compressive and Shear forces placed into the body did transmit into deeper tissues. As with the American study, the shear displacement was less in the deeper tissues than in the superficial ones, but this would be expected as forces applied to the body would be expected to dissipate as they travel deeper into the tissues of the body. Therefore, it is reasonable to assume that these forces could plausibly affect underlying bones (spinal vertebrae).
How Might This Occur?
Displacements of tissues most likely arises passively, consistent with load transmitted by the retinacula cutis and epimuscular force pathways. “Retinacula cutis” is a complex of fibrous structures that traverse the subcutaneous fat linking the skin to the deep fascia and capable of transmitting loads from multi-directional forces (in other words loads that are not perfectly compressive/ perpendicular).
So What Does This All Mean?
It would seem that taking any theory or ideology too far is dangerous. Certainly, the interfaces of soft tissues of the body are quite slippery, in other words, have very little friction. After all, they are meant to be sliding surfaces. However, they are not perfectly frictionless so oblique forces (that are not perfectly perpendicular) can transmit into deeper tissues. Further, as stated above, the oblique force should be able to be resolved into its perpendicular (compressive) component. And once the slack of the more superficial tissue has been removed, then that tissue being tensioned should transmit that tension into the underlying structures, likely the underlying bone. Certainly, the magnitude of the force transmission does decrease as it travels deeper into the body, but it does transmit. Both direct and indirect stimulation of mechanoreceptors of tissues across both depth and breadth is possible.
This article is written in collaboration with Dr Joe Muscolino, www.learnmuscles.com